8
March

With one of the top PharmD programs in the nation, the School of Pharmacy excels in preparing graduates to thrive in residencies
By Katie Ginder-Vogel
Between 2013 and 2021, applicants in the American Society of Health-System Pharmacists (ASHP) Residency Match program have increased 63 percent, but because positions in residency programs are limited, matches haven’t grown at the same rate. In the same time frame, the number of unmatched applicants has grown by 52 percent.
Residencies aren’t a requirement for all pharmacy careers, but many graduates who want to go into a specialty or secure a leadership position choose to apply to residencies to expedite that process and build expertise.
Nearly half of UW–Madison School of Pharmacy PharmD graduates pursue residencies, and despite the rapid growth in applicants nationwide, the School continues to have one of the highest residency match numbers in the nation. In 2020, the School had the fifth-most student pharmacists matched to residencies, and in 2021, 84 percent of the School of Pharmacy’s applicants matched with residencies, compared to a national average of 67 percent.
“We have built a core curriculum and curricular paths within the PharmD degree that focuses on improved patient-centered care, which helps student pharmacists develop leadership skills, sharpen their problem-solving abilities, and longitudinally advance the growth of their clinical judgment,” says Professor Mel de Villiers, associate dean of academic affairs at the University of Wisconsin–Madison School of Pharmacy. “These skills are essential as the profession of pharmacy moves toward a more patient-centered, clinical focus. The evidence that this approach is working is shown by our student’s success in obtaining residencies.”
“Research skills and clinical practice are two large components of residency training, and the UW–Madison School of Pharmacy PharmD program is exceptionally strong in both areas.”
—Paria Sanaty Zadeh
School of Pharmacy alumni have used their residencies to find careers informing drug policy at the National Institutes of Health, hospital pharmacy supervision, supply chain informatics, national pharmacy leadership, and more, and credit the School’s PharmD program as a launchpad to their success.
“Research skills and clinical practice are two large components of residency training, and the UW–Madison School of Pharmacy PharmD program is exceptionally strong in both areas,” says Paria Sanaty Zadeh (PharmD ’17), associate director of practice and science programs at the American Pharmacists Association. “The School pushed me to adopt a scientific mind and advance my patient care skills to become a well-rounded pharmacist practitioner who was highly qualified and prepared for a challenging residency program.”
Drug policy at the National Institutes of Health
In her fourth year of pharmacy school, Mary Frances Picone (PharmD ’16) met her mentor, Megan Holsopple, during a rotation with the Center for Medication Utilization at Froedtert Hospital in Milwaukee, which helped her decide that drug information could bridge her interests in clinical practice, academia, and research.
As a PharmD student at the School of Pharmacy, Picone opted for the Residency Track Advanced Pharmacy Practice Experience (APPE RT) in her fourth year of the PharmD program, which is spent entirely on clinical rotations in a variety of practice environments. Through the APPE RT, she spent six months exploring different areas of Froedtert Hospital and gained an in-depth understanding of how that health system operates, which enables a higher level of student contributions.

“It was a longitudinal APPE, with four of six clinical rotations at the same hospital, almost like a ‘mini residency’ in my fourth year,” Picone says. “They were focused rotations in different areas of the hospital, such as medication utilization, and we were assigned a longitudinal project meant to introduce what might be expected of us as residents, managing rotations and longitudinal responsibilities throughout an entire year.”
Following her rotation with Holsopple, Picone applied and was matched to a two-year specialty residency at the Medical University of South Carolina. The first year was focused on acute care pharmacy with the benefit of being able to complete several electives within her future specialty area. During her second year, she was able to build upon those introductory experiences to develop expertise in drug information, ultimately working toward leading her own projects, teaching students and PGY1 residents, and functioning independently as a drug information specialist.
After her residency, she returned to Froedtert to work full-time as a medication utilization pharmacist and the PGY-2 drug information residency program coordinator, with Holsopple as her supervisor.
The interest and experience she gained through her APPE RT, subsequent residency, and role with Froedtert would lead her to her current, far-reaching position: drug information/drug policy officer at the National Institutes of Health (NIH) in Washington, D.C.
Picone’s role at NIH is similar to drug information and medication use policy roles in other organizations, but with a unique population.
“Our clinical center is America’s research hospital; all patients being seen at the hospital are on a clinical trial,” explains Picone. “Managing the formulary, which primarily focuses on reviewing medications available for use as standard or supportive care, while accounting for the fact that the formulary needs to support the integrity of study protocols, is the most interesting and challenging part of my job.”
Additionally, the mission of NIH is to fund research in under-studied areas, often including patients with rare or undiagnosed diseases, which challenges the population health concept for the formulary.
As part of her role, she serves as secretary of the Pharmacy and Therapeutics (P&T) Committee, which is the group responsible for reviewing proposed changes to the formulary, or the list of medications available for use in the hospital to make sure medications are being used in a safe, effective, and fiscally responsible way. The Committee reviews all formulary changes, including requests from prescribers to add new medications to the list, and makes changes to ensure the optimal use of available medications.
“UW provided numerous professional engagement and leadership opportunities that promoted a sense of getting involved very early in my education.”
—Mary Frances Picone
Picone also runs the Drug Information Service, a service available to physicians, staff, and patients to answer complicated medication-related questions, managing medication-use policies and guidelines to support the aim of P&T and ensure compliance with regulatory standards, and communicating the work of the P&T Committee by maintaining available resources and distributing monthly updates.
Picone credits the well-rounded education she received at the School of Pharmacy, coupled with student resources like mock interviews and resume preparation, with giving her the tools to get where she is today.
“UW provided numerous professional engagement and leadership opportunities that promoted a sense of getting involved very early in my education,” Picone says. “I built upon that in residency and my subsequent professional positions.”
Compounding and hazardous drugs
As a PharmD student, Nate Menninga (PharmD ’17) also completed the APPE RT, at UW Health in Madison, and worked with John Dopp, associate professor in the Pharmacy Practice Division, on research.
“Dr. Dopp introduced me to the lung transplant team that I worked with during my residency, and we still talk to this day,” says Menninga. “Residency is competitive, and my work with Dr. Dopp, including publications and other stories, personalized my application.”

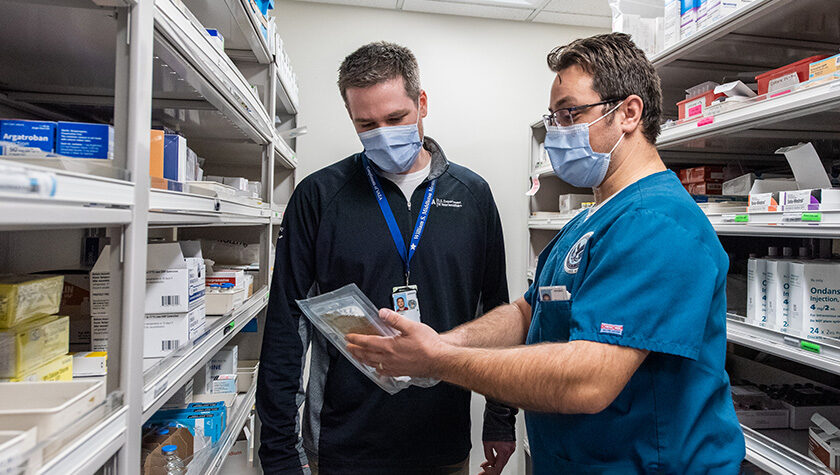
Menninga matched with a residency at the William S. Middleton Memorial Veterans Hospital in Madison, where he is now the pharmacy supervisor of compounding and hazardous drug programs.
“Residency bridges the gap between didactic learning and delivery of health care and provides a foundation of clinical experience and, more importantly, an understanding of how health care is delivered to a patient — how clinical decisions get transformed into patient care,” Menninga says. “If a provider wants to change an insulin dose, what needs to happen? You need to know how many vials and syringes the patient gets, what the instructions on the label say.”
In addition to providing research and longitudinal APPE opportunities, Menninga says the School of Pharmacy also gives student pharmacists a solid foundation of clinical knowledge and skills to evaluate literature, explore guidelines, and use clinical tools to be effective in a fast-moving field.
“When you get into residency and practice, new literature guidelines keep coming,” Menninga says. “The School gives you the skills to figure it out on your own and decide for yourself what a patient might need.”
Menninga also cites the mock patient interactions in the School’s Pharmacist Communications course, which helps students practice interacting with patients and other clinicians.
“As we move toward team-based practice models, students need that baseline communications training to deliver healthcare in a residency setting,” he says. “As a pharmacy student, I remember my interactions with residents from area programs who came to the School to be patients or preceptors, and I remember interacting with practicing pharmacists, fresh into their careers, and getting their feedback about specifically how to make an interview flow better.”
Informatics and supply chain
During his residency at UW Health, Randy Braun (PharmD ’16) was tasked with implementing an IV to oral medication guideline for use in American Family Children’s Hospital in Madison. In the second year of his residency, focused on informatics, his project was to reimagine how pharmacists documented their patient monitoring, which was implemented in 2018. However, it was the projects and rotations in supply chain during the second year that really piqued his interest.
“I got exposure to areas I didn’t know existed, like supply chain,” says Braun. “Residency gives you a greater depth of participation in patient health care and helps change how pharmacy care is delivered.”

That residency experience has helped Braun become the informatics pharmacist coordinator at UNC Health in Chapel Hill, North Carolina, where he works with the pharmacy supply chain management group. Braun’s team manages the software they use to do inventory management, procurement, and orders management from Epic for patient orders in the hospital network. They also manage the automation hardware at the health system’s consolidated service center — four carousels where the health system stores medications.
“We have various pieces of automation, which augment the pharmacist and technician roles in the medication use process,” Braun adds. “When a new hospital went live recently, that previously had no automation, we were able to implement the dispensing software so when patient orders come in from the electronic health record, the technicians and pharmacists utilize the software and automation to make their work safer and more efficient. I love it.”
Braun’s team is also charged with ensuring compliance with the Drug Supply Chain Security Act (DSCSA) for electronic, interoperable product tracing from the manufacturer to the patient’s bedside, to make sure no counterfeit meds make their way into the supply chain.
“Supply chain pharmacy to me is fascinating,” he says. “It isn’t the same close patient interaction I enjoyed during residency, but it is an opportunity to solve complex problems, save the healthcare system money, and create efficiencies while impacting patient care at the system level.”
Braun’s residency was critical in getting him where he is today, and he says it all traces back to the rigorous academics, high-quality clinical experiences, and supportive environment — including mentors Professor Mel de Villiers and Associate Professor Karen Kopacek — at the School that set him up for residency success.
“The people make a place, and there are so many helpful, good people at the School of Pharmacy,” Braun says. “I feel very fortunate that I was able to experience the things there that shaped me as a person and paved the path to residency.”
Leadership with a national scope
Like Braun, Paria Sanaty Zadeh is not working directly in patient care. Instead, she’s shaping pharmacy practice at a higher level, as the associate director of practice and science programs at the American Pharmacists Association (APhA).
“I felt like this job description was written for me,” she says. “I’m not in frontline pharmacy practice, but I use my intimate knowledge of pharmacy practice every day in my work and draw on all my clinical skills.”
At APhA, she is responsible for elevating and advancing pharmacist patient care services and serves as the APhA liaison between the association’s members and leaders.
“I wanted to merge clinical practice and leadership, so I did two years of residency, the first year in hospital pharmacy practice, to learn how to be a strong pharmacist before managing people, and the second year in health system pharmacy administration leadership, as well as the ASHP Pharmacy Leadership Academy,” she says.

She laid the groundwork for her residency through the APPE-RT and multiple leadership experiences at the School of Pharmacy, such as with the Interprofessional Health Council (IPHC), MEDiC student-run clinics, and the Wisconsin Area Health Education Centers (AHEC).
“Participating in developing therapeutic plans at MEDiC with other health profession students and a licensed practitioner preceptor was an invaluable experience in preparing me for residency rotations, especially those in ambulatory care,” she says.
Sanaty Zadeh was invited to interview at all the residency programs she applied to, and matched with her top choice, Beaumont Health in Detroit, Michigan, which she says is a testament to the UW–Madison School of Pharmacy experience.
“It all goes back to a rigorous curriculum, plethora of research opportunities, variety of extracurricular activities, world-class faculty, and top-notch mentoring,” she says. “On top of all of this, the School upholds a culture of excellence for high-quality work and high-level thinking and is always fostering the Wisconsin Idea — stimulating curiosity, exploration, and an expansive mindset of learning and impact beyond the boundaries of the classroom.”
Recently, Sanaty Zadeh was charged with launching the APhA Academy of Pharmacy Practice and Management Pharmacy Residency Standing Committee, which offers informational resources and networking to help pharmacy residents and fellows across the country maximize their postgraduate experiences.
“It is surreal, now being on the other side of the residency experience as I support APhA’s PGY-1 Community-Based Pharmacy Residency Programs nationwide, which APhA jointly accredits with ASHP,” she says. “Through this work, I have gained an even greater appreciation for the standards and principles that the School instilled in me as a pharmacy learner.”