Meet recent School of Pharmacy alumni who are leading their fields forward
By Katie Gerhards
We know our Pharmacy Badgers are movers and shakers — we see it in each edition of Class Notes. That’s why we wanted to create a new annual feature highlighting some of the tremendous accomplishments by recent alumni from each of our degree programs: Bachelor of Science in Pharmacology and Toxicology (PharmTox), Doctor of Pharmacy (PharmD), Master of Science in Health System Pharmacy Administration, PhD in Health Services Research in Pharmacy (HSRP), and PhD in Pharmaceutical Sciences (PharmSci).
From guiding Wisconsin pharmacy practice into the next era to improving lives and shaping policy in Cambodia, these impressive alumni have graduated within the last 15 years and have left an indelible mark on their fields. Meet the University of Wisconsin–Madison School of Pharmacy’s 2021 Five of the Future.

Location: Washington, DC
Position/Employer: Research and Learning Advisor, Program Cycle Specialist at Social Solutions International
Claim to Fame: Shaping social, economic, and health strategies around the globe.
Proudest moment: His first main-author publication, part of his dissertation, was featured on the cover of the journal Clinical Cancer Research.
Inspiration: “I have to work in a field that I believe helps people in some way.”
Graduates of the School of Pharmacy’s Pharmacology and Toxicology bachelor’s degree program are set up for a breadth of careers, with alumni who have gone into research, healthcare, and even law. Even among that diverse group, the career of PharmTox alum Derek Simon (BS ’06) stands out.
Simon was one of the forces behind the development of Cambodia’s Country Development Cooperation Strategy (CDCS), which is essentially the United States Agency for International Development’s (USAID) five-year plan for programming. As an institutional support contractor for USAID, he had been living abroad in Cambodia to support the CDCS development, until COVID-19 pushed him back to the U.S. about a year ago.
“I was living in Cambodia for a year to help conduct a country-wide learning and research project in preparation for their new strategy that would outline the types of programs that would be done to support the Cambodian people over the next five years,” he says.
“It’s all about problem-solving — how to take a topic you don’t know about and figure out solutions to it, and that’s what I’m doing at USAID.”
—Derek Simon
To start this plan, which spans December 2020 to December 2025, they needed an in-depth and comprehensive analysis of the country’s challenges and opportunities.
“They wanted to specifically hear from rural and marginalized communities,” he says, which required travel throughout the country.
To inform the creation of the CDCS, Simon organized research projects, helped with the analysis, and trained staff to do data collection, such as qualitative interviewing. With data in-hand, the next step was to develop the strategy itself, which was a long process that required a series of workshops and the completion of three formal phases outlined by USAID headquarters in Washington, DC. The final product has three objectives: to have inclusive and sustainable economic growth broadened; health, education, and welfare of Cambodians improved through enhanced services; and human rights protected and government accountability advanced.

“It was very satisfying to finally have the formal approval of the final document,” says Simon. But what he found most satisfying was the completion of the final report that summarized the team’s stakeholder consultation work.
“While the CDCS was a large group effort that I was heavily involved in, the stakeholder consultation report was entirely drafted by me, so it was the most direct output from my work with Cambodia,” he says.
He also developed two guidance documents based on this work, to share best practices and learning with USAID.
With the plan itself created and released, Simon’s attention now turns toward monitoring, evaluation, and learning.
“We’ve been defining the set of indicators and other tools that will help us measure progress toward this strategy over the next five years and make sure that it’s been implemented effectively,” says Simon.
How does a PharmTox alum — with a PhD in cellular and molecular biology — come to shape social, economic, and health strategies around the globe?
“It’s a bit unusual,” Simon says.
After earning his PhD from the University of Michigan, Simon was completing a postdoctoral fellowship focused on the neuroscience of drug addiction at the Rockefeller University in one of the labs that pioneered the use of methadone as a treatment for opioid misuse. Looking for his next opportunity, and hoping to explore other facets of the opioid epidemic, he applied for a fellowship through the American Association of the Academy of Sciences (AAAS). The two-year AAAS Science and Technology Policy Fellowship — which places scientists and researchers in a government office to learn more about policy and governmental functions — seemed like a promising avenue to find new terrain.
“Surprisingly, none of the program descriptions for that year were dealing with opioids, so I had to adjust and think about something else to work on,” he says.
He landed on something unexpected: a USAID office working on LGBTI (lesbian, gay, bisexual, transgender and intersex) issues and improving the inclusion of marginalized groups into USAID programs. It was a 180-degree turn from his formal training, but he was excited for the new challenge and the opportunity to improve people’s lives in a different way.

“After the two years of the fellowship, I knew I wanted to stay at USAID, but I wanted to do something more aligned with my science background,” he says.
Although there is no benchwork with his USAID/Cambodia role, the research, monitoring, and evaluation he’s working on still allows Simon to stretch his scientific legs and use the foundation of analytical thinking that he honed during the PharmTox program.
“Getting the research exposure that I did at UW–Madison was one of the most valuable things,” says Simon. “It’s all about problem-solving — how to take a topic you don’t know about and figure out solutions to it, and that’s what I’m doing at USAID.”
As his current project with USAID/Cambodia wraps up, he’s eyeing a pivot back into the hard sciences and biotechnology. Although he doesn’t want to delve back into full-time benchwork, he is drawn to the technical challenges of the field and is spurred on by the rush of science surrounding the pandemic.
“I couldn’t help but think that if I had remained in my original field, I might have been involved in some type of work that could have contributed to fighting COVID-19,” he says. “My ‘first love’ was always science.”
Back to top

Location: Beaver Dam, Wis.
Position/Employer: Director of Clinical Services, Hometown Pharmacies
Claim to Fame: Pushing pharmacy practice forward by innovating comprehensive, patient-focused services.
Inspiration: “I’m really motivated by helping pharmacies shift to provide new, essential services in a sustainable way.”
Proudest moment: Every time she helps a patient make lifestyle changes to overcome the need for medication.
As a PharmD student at the School of Pharmacy, Abbi Linde (PharmD ’11) said she was going to be the pharmacist who got her patients off their medications. At the time, she had intended to do that by helping to deprescribe patients from redundant or outdated medications.
Now that she owns her own pharmacy — Hometown Pharmacy in Beaver Dam — the end goal is the same, but she’s accomplishing it by partnering with patients to change their lifestyles and make medication therapy unnecessary.
“Every time I help someone not need a medication, that makes my heart so happy,” she says. “For that person’s life, that’s a huge deal.”
Linde is currently working toward a certification from the Institute of Functional Medicine, which will complement her qualifications as a certified health coach and primal health coach and further empower her to address patients’ foundational health.
“Every time I help someone not need a medication, that makes my heart so happy. For that person’s life, that’s a huge deal.”
—Abbi Linde
Some alternative medicines have claimed the title “functional medicine,” but true functional medicine — which is even being embraced by the National Community Pharmacists Association — is evidence-based and addresses the underlying causes of diseases and symptoms by considering sleep, diet, stress, and other factors.
“As a pharmacy student, I did an independent study with Professor Beth Martin about nutrition and motivational interviewing,” says Linde. “I think it’s so funny that I came back to that so strongly later in my career, but at the time I had no idea.”
For example, Linde’s Hometown Pharmacy is a supplier for the Medicare Diabetes Prevention Program, which is a Centers for Disease Control-recognized lifestyle program that has proven to be twice as effective as metformin in preventing or delaying the onset of diabetes.

“We’re in the process of establishing as a hub so that we can support other pharmacies in Wisconsin to provide the service,” she says.
They are also creating a diabetes self-management education program and have run programs to guide patients through weight loss and elimination diets, which can identify food sensitivities.
“We also do supplement reviews, helping patients make sure that the supplements they’re taking are safe, effective, and from a quality brand,” she says.
Linde’s pharmacy also launched a program called “Educate, Empower, Evolve,” that focuses on helping patients improve six metrics — such as waist-to-hip ratio, blood pressure, and vitamin D levels — that will reduce their risk of disease and illness.
“We’re really trying to shift to a business model where we are getting reimbursed for our services primarily, and the medications are secondary,” she says.
When Linde purchased the Hometown Pharmacy in Beaver Dam four years ago, she set a goal: to become the director of clinical services for all 72 Hometown Pharmacy locations within five years.
“It wasn’t even a position that existed within Hometown,” she says. “I was working hard to implement new services in the Beaver Dam pharmacy, and I really wanted to help other stores do the same thing.”
Linde achieved her goal with time to spare, and for the last year and a half, she has been working with pharmacists throughout the Hometown Pharmacy network on services like medication synchronization and comprehensive medication reviews.

But her work to advance practice and help pharmacies launch innovative services transcends Hometown Pharmacies and reaches all corners of Wisconsin: Linde is a luminary for the Community Pharmacy Enhanced Services Network (CPESN) luminary and a coach for Flip the Pharmacy, which is a CPESN initiative that helps pharmacies transform their services.
“Each month there are different tasks and focuses, and my job as a coach is to help make sure that our stores are following along, address any barriers and challenges, and provide positive reinforcement,” she says.
The Wisconsin CPESN is an access point for its 63 member pharmacies to access a supply of COVID-19 vaccinations, which Linde coordinated.
For how much she’s already accomplished, Linde has even more planned for the future. She will continue to transform her pharmacy into a wellness center and build up her team and services at Beaver Dam, freeing up more of her time to help other pharmacies do the same. But she may also take some time to get re-acquainted with her inspiration: her patients.
“I’ve had a calling on my heart lately to get back to working directly with patients,” she says. “I love to hear how we’ve changed their lives.”
Back to top
Position/Employer: Research Assistant Professor, University of Michigan College of Pharmacy
Claim to Fame: Using automation and artificial intelligence to improve patient safety and pharmacist workflow.
Inspiration: “I like to help people and work on intellectually challenging problems that can be disseminated to affect a broad group of patients.”
Proudest moment: Having his application for an R01 grant from the National Institutes of Health ranked in the top 6 percent.
“The idea is to think about our automation or artificial intelligence as a team member in the pharmacy,” says Corey Lester (MS ’15, PhD ’17).
As a research assistant professor at the University of Michigan College of Pharmacy, Lester and his research team are building predictive models to leverage what computers do well — processing large amounts of data and perform routine tasks consistently — to support pharmacists.
One area in particular that Lester is working on deals with electronic prescription directions.
“Prescription directions come into the pharmacy from the prescriber, often poorly written in jargon, and pharmacists have to unpack, edit, and translate the intent of those directions,” says Lester, who is being promoted to tenure-track assistant professor in July 2021. “That takes time and effort, and people are prone to mistakes that can result in patients taking their medication differently than intended.”
In order to prevent errors, it’s a two-step process, where one staff member edits the directions, and another verifies that they were edited correctly. Lester’s solution is a computer model that can predict how pharmacy staff would have interpreted the original directions, reducing the amount of repetitive work for pharmacy staff. The model would take the first pass at the directions, and a pharmacist would verify the edits.
“Publications don’t excite me as much as hearing about people reading about my work and making changes to their own practice because of it.”
—Corey Lester
“As the pharmacist corrects them, it will teach the model how to do better in the future,” he says.
A second area that Lester is exploring is how pills are bottled for individual prescriptions. Using an image of the pills or capsules inside the bottle, he’s building a computer model intended to identify those medications and when the bottle has been filled incorrectly — such as if an extraneous pill made it into the wrong bottle.
While building these models and interventions, Lester is also keeping an eye on what their implementation will do for patient outcomes and pharmacist workflow.
“We also have to keep in mind how these tools might augment pharmacists’ cognitive work,” he says. “While the goal is to enable them to take on new clinical tasks and patient services, if the models are used inappropriately they can lead to unintended consequences for patient safety.”
Lester’s automation innovations haven’t yet been implemented, but he’s drawing closer through promising applications for R01 grants from the National Institutes of Health to test their effects on patient safety and pharmacist work in laboratory settings — which is highly competitive funding and nearly unheard of in health services research in pharmacy.
He has recently submitted two R01 applications, which were ranked in the sixth and fifth percentiles, highlighting his work’s value and the strength of his approaches and research proposal. Since 2020, he’s also published 10 research manuscripts, including in the BMJ Quality and Safety, Journal of the American Pharmacists Association, and JMIR Medical Informatics

When he first became interested in leveraging data to improve patient outcomes, Lester was completing a PGY-1 residency at Virginia Commonwealth University after earning his PharmD from the University of Rhode Island.
“That’s what drove me to Wisconsin. I wanted to develop my skillset of analyzing medication data and how it leads to new knowledge that can be used to advance patient care,” he says. When searching for graduate programs, he met with Professor Michelle Chui, chair of the School’s Social and Administrative Sciences Division, who is steeped in systems engineering approaches to problem solving. “That mindset and approach were really appealing to me.”
Additionally, Lester was looking forward to the opportunity through the School’s Social and Administrative Sciences in Pharmacy program (now Health Services Research in Pharmacy) to explore classes outside of the School of Pharmacy, in math or engineering.
“I felt that there was a huge benefit going outside of pharmacy to learn about engineering theories and statistical methods that could be brought back, applied to pharmacy practice, and connect them to my own work,” he says.
Now four years out of Chui’s research group, he continues to lean on her for occasional support and advice.
“I really value that relationship and I owe a lot to her for the effort that she put into my grad school career and setting me up well to start my career at Michigan,” he says.
In planning his next career moves, Lester is hoping to build a research center focused on developing and testing tools to improve patient care and pharmacists’ work.
“I want to feel like I’ve actually made a difference,” he says. “Publications don’t excite me as much as hearing about people reading about my work and making changes to their own practice because of it.”
Back to top
Position/Employer: Assistant Professor of Chemistry, George Washington University
Claim to Fame: Developing mass spectrometry-based tools to understand brain diseases.
Inspiration: “I’m a curiosity-driven person; discovering the unknown is intrinsically what excites me.”
Proudest moment: Starting and building her own research group at George Washington University.
The average age for a PhD scientist to receive an R01 grant from the National Institutes of Health (NIH) is 43. When Ling Hao (PhD ’17) received her first R01, as an assistant professor at George Washington University, she was just 29.
It’s been four years since Hao graduated from the School of Pharmacy, and she has already published 25 peer-reviewed articles, landed a five-year R01 grant from the NIH, and has established her own research lab with a growing team of six. She was honored in 2020 with a Ralph E. Powe Junior Faculty Enhancement Award from Oak Ridge Associated Universities, and she’s served as a reviewer for 15 journals focused on chemistry and biomedical sciences.
What is her secret to success? It’s a combination of mentor support, careful planning, and devoting time to her personal hobbies.
At the School of Pharmacy, Hao studied in the lab of Professor Lingjun Li, who remains a close mentor and colleague.
“She is definitely the most supportive PI [principal investigator] in the world,” she says.
In the Li Lab, Hao learned a variety of mass spectrometry techniques and other research skills that she continues to use today, and she also began to envision her future academic career.
“Learning should be a lifelong journey, and it should be fun and inspiring.”
—Ling Hao
“During my PhD, I started to think about what labs need and what I would do if I were the PI,” she says. “I think one of the reasons I got my lab started so smoothly is because I’d been thinking about this for several years and learning from various mentors.”
The Li Lab helped her get acquainted with the logistics of managing a large team and running a well-established lab. After graduating from the School of Pharmacy, during a postdoctoral fellowship at the National Institute of Neurological Disorders and Stroke, she worked with both a senior advisor (Richard Youle) and a junior advisor (Michael Ward), where she learned how to hire lab members and set up a new lab from scratch.
When it came time to set up her own lab at GWU, she was prepared to hit the ground running. Within a year of starting the Hao Lab, she’d attracted two graduate students and two undergraduate students. With their help, she’s working on her new R01 grant to develop mass spectrometry strategies to decipher the dynamic lysosomal dysfunctions in frontotemporal dementia — the most common form of dementia for people under age 60.
“The human brain is perhaps the most mysterious part of the human body,” she says. “After decades of drug development, most of the brain diseases are still incurable, and a main reason is we don't understand the brain enough, especially the molecular processes underlying the disease processes.”
Lysosomes are organelles in cells that is essentially in charge of trash disposal, Hao says. If lysosomes aren’t functioning properly in the brain, cellular trashes accumulate and stress up the brain.
“That’s actually one of the hallmarks of neurodegenerative disease,” she says.
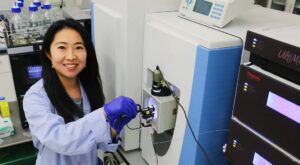
But because it’s so dynamic, the microenvironment and cellular interactions of lysosomes are not well understood yet. Mass spectrometry techniques provide a high-throughput, unbiased, and quantitative way to look at the lysosomal microenvironment in neurons — a method she established in an earlier paper, published in Analytical Chemistry. Now with the R01 grant, she can further develop the method and apply it to understand the molecular mechanisms behind neurodegeneration.
“I want to develop really cool mass-spec methods to make available to the scientific community to overcome technical challenges and decipher mechanisms that underlie neurodegenerative diseases and better understand the human brain,” she says. “This field has many unmet needs and exciting but unknown aspects that need to be studied.”
While she’s excited to continue to build her research program, she’s also grateful for the opportunity to influence the education of budding researchers as both a professor and mentor.
“I think the most rewarding part of being a PI, sometimes even more rewarding than scientific achievement, is to see the growth of the students and feel their excitement about research and their accomplishments,” she says. “I am really lucky that all my previous mentors are very supportive, which has motivated me to become a good and caring mentor to benefit more students.”
She also teaches two chemistry courses, which allows her to reach more students and build her own skills in science communication.
“One of the things I learned from my parents, which continues to influence me, is that learning should be a lifelong journey, and it should be fun and inspiring,” she says. That’s why she leaves room in her life to explore a breadth of hobbies and experiences.
“I like traveling, I love cooking — I’m really a foodie — and I love music and singing,” she says. “These kinds of things in my life make it more colorful. I like that every day could be a different day.”
Back to top

Location: Boston, Mass.
Position/Employer: System Executive Director, Ambulatory Pharmacy Services, Wellforce
Claim to Fame: Transforming and advancing health-system pharmacy at local and national levels, while sharing her enthusiasm, passion, and expertise.
Inspiration: “Talking with my team members about their favorite patient stories and how they made a difference in their care by sharing the medication expertise. It inspires me to continue developing clinical programs and services and improving systems to better serve our patients.”
Proudest moment: Justifying and implementing emergency medicine pharmacy services at Tufts Medical Center.
Melissa Ortega (MS ’12) has spent the entirety of her nine-year career within the Tufts Medical Center. And all the while, she’s been growing as a leader, introducing new clinical programs, and changing the lives of Tufts’ patients. Soon, she’ll be doing the same across the Tufts health system’s three hospitals.
She started out as a manager within the central pharmacy at Tufts Medical Center, overseeing medication use processes for acute care, and she hit the ground running.
“I was excited to implement technologies within each phase of the medication use systems that not only allowed safe medication practices but also allowed us to advance pharmacy technicians’ roles,” she says.
They created a team-based technician model in which technicians practiced at the top of their license as pharmacist extenders and helped collect medication histories. Additionally, she enhanced the sterile products area services by expanding hours, insourcing, preparing more ready-to-administer doses, launching quality assurance programs, and implementing barcode medication preparation technology.
“I really came to realize how much I love pharmacy leadership and different aspects of impacting patient care through program development and building teams.”
—Melissa Ortega
“It was a very busy first couple of years — almost like another residency admin program,” she says.
She then moved on to become the director of inpatient pharmacy operations and pediatrics, where she expanded pediatric and emergency medicine clinical pharmacy services. Within the last four years, she’s been translating those skills and experiences as the director of ambulatory pharmacy services at the hospital.
“Over the past few years, we’ve spent a lot of time understanding how pharmacy services can add value and drive outcomes where we have high-risk patients on complex, chronic, and costly medications and have prioritized those clinics to provide pharmacy services,” Ortega says, which has led her team to expand pharmacy services to nephrology, pediatrics, primary care, endocrinology, and pulmonary departments.
Her team focuses not only on making sure that patients can access and afford their medications, but also on making sure that they’re appropriate and patients are benefiting from them and achieving their care plan goals. In many cases, such as those involving prior authorization for prescriptions, the pharmacy team does follow-ups with patients to monitor outcomes, adherence, but most importantly establishing the longitudinal relationship with the patient. In their unique model, pharmacists are integrated within care teams and are accountable for medication outcomes.

Recently she was promoted to lead ambulatory, specialty, and retail pharmacy services for the whole health system, which includes Tufts and two additional community hospitals: MelroseWakefield Hospital and Lowell General Hospital.
“As a profession, we are one of the most accessible health care providers in the community, and I am honored to continue to innovate and lead our ambulatory pharmacy services to be there for all our patients’ medication needs,” Ortega says.
Ortega’s interest in health-system leadership and clinical service innovation came as an unexpected turn during her fourth-year rotations as a student pharmacist at Nova Southeastern University in Florida.
“I really came to realize how much I love pharmacy leadership and different aspects of impacting patient care through program development and building teams,” she says. But her home state of Florida didn’t have any administrative residency programs or training available in pharmacy leadership at the time.
“It was a blessing in disguise because this really challenged me to venture outside of my comfort zone,” she says.
At an annual Florida Society of Health-System Pharmacists meeting, she met Steve Rough (BS ’91, MS ’94), then the director of the Health System Pharmacy Administration residency program at UW Health, which is a joint master’s degree program at the School of Pharmacy.
“I was immediately attracted to the values of the program at Wisconsin and could clearly see the passion for a patient-centric approach to leadership and decision-making,” she says. “That took me to a very different climate up in Madison, and the rest is history.”
Ortega’s career and contributions to the field transcend Tufts and associated hospitals, including statewide leadership as the past president of the Massachusetts Society of Health-System Pharmacists and shaping national practice through various committees of the American Society of Health-System Pharmacists (ASHP).

She’s been an active advisory group member in the ASHP Section for Specialty Pharmacy Practitioners and is currently chair of the ASHP Section of Community Pharmacy Practitioners and a member of ASHP’s new Racial Diversity, Equity, and Inclusion Task Force.
“I wanted to give back and be a part of the solution for what was facing so many minorities within our country — and what better way to really understand that for not only our profession but for our patients,” says Ortega, who also serves on Tufts’ Diversity, Equity and Inclusion Committee. She’s now also working with other Badger alumni of the Health System Pharmacy Administration program to develop a mentorship program for minority pharmacy residents.
“It’s brand-new, but we thought this would be a great way to reach out to minority pharmacy residents and do more formal mentorship to provide the support that I know I was fortunate to get,” Ortega says.
Her years of service to ASHP and the profession have also earned her the honor of being a 2021 Fellow of ASHP — in her first year of eligibility.
“I feel like I’ve been able to make what I call the Badger footprint in the lives of patients that we care for here in Boston,” she says. “I really owe a lot of what I’ve been able to accomplish to all of my mentors, teachers, and Badger training — on Wisconsin!”