This is an accordion element with a series of buttons that open and close related content panels.
Why is establishing an opioid stewardship leadership team important?
Establishing an opioid stewardship leadership team, such as a committee or task force, within the health system is important. This team can help to raise awareness, strategize the top priorities for the organization, establish goals, and drive progress related to opioid stewardship.
Committees/task forces that are comprised of leadership or executives can be beneficial and will be able to:
- Provide top-down structure to legitimize opioid stewardship efforts,
- Provide high-level direction, organization, guidance for projects across the health system,
- Ensure opioid stewardship work across the health system is a priority,
- Encourage and facilitate collaboration on opioid stewardship, and
- Address challenges to making progress with opioid stewardship efforts. (Weiner, 2018)
Committees/task force membership should also include frontline staff (e.g., staff who are directly involved in providing care every day), who provide an on-the-ground perspective of the critical details and logistics necessary for the success of opioid stewardship activities.
The importance of establishing an opioid stewardship committee or task force is reflected in national quality, accreditation, and regulatory authorities’ recommendations or requirements to form a leadership team focused opioid stewardship:
In 2018 & 2019, the Joint Commission released new and revised Pain Assessment and Management Standards for hospitals, critical access hospitals, and ambulatory care organizations. Each standard has a similar new requirement that these organizations must have a leader or leadership team that is responsible for opioid stewardship-related activities.
Requirement – EP 1: The hospital has a leader or leadership team that is responsible for pain management and safe opioid prescribing and develops and monitors performance improvement activities.
Leadership responsibilities for developing and monitoring performance improvement activities specific to pain management and safe opioid prescribing
Whether an individual ‘leader’ is assigned this responsibility, or a ‘leadership team’ model is used, responsible leader(s):
- participate in defining the goals and metrics for performance improvement activities, e.g., on monitoring the use of opioids;
- allocate resources to conduct performance improvement activities;
- review performance improvement data;
- promote improvement in practices and accountability across disciplines and services involved in pain management and opioid prescribing
The Centers for Disease Control and Prevention (CDC) published a guide for implementing the 2016 CDC Guideline for Prescribing Opioids for Chronic Pain which included guidance related to opioid stewardship committees or task forces.
 If your practice or system has the resources and is able to create a change team, they can be responsible for the next steps, including implementing and monitoring the changes. The team should be interdisciplinary and should consist of leaders and staff. It is important to have clear roles for the champion and other change team members. Ideally, the team will include a range of roles, all of which will be involved in the change effort (e.g., medical directors, clinicians, nurses, medical assistants, pharmacists, behaviorists, clinical and/or front office staff managers, case workers). Consider representation from other key areas, such as IT, as many of the practice recommendations involve creating workflows within an EHR and pulling reports for clinical QI measures.” (CDC, 2018)
If your practice or system has the resources and is able to create a change team, they can be responsible for the next steps, including implementing and monitoring the changes. The team should be interdisciplinary and should consist of leaders and staff. It is important to have clear roles for the champion and other change team members. Ideally, the team will include a range of roles, all of which will be involved in the change effort (e.g., medical directors, clinicians, nurses, medical assistants, pharmacists, behaviorists, clinical and/or front office staff managers, case workers). Consider representation from other key areas, such as IT, as many of the practice recommendations involve creating workflows within an EHR and pulling reports for clinical QI measures.” (CDC, 2018)In a 2020 publication focused on opioid stewardship measurement, the American Hospital Association (AHA) reiterates the Joint Commission requirements and offers the following considerations:
“Considerations for Forming a Leadership Team
- Executive leadership. Create an executive leadership team that includes chief medical or quality directors. Sponsorship from executive leadership demonstrates organizational priority and can assist when resources or funding is needed.
- Multiple service lines/departments. Leaders with responsibilities across departments or service lines provide a broad line of sight, which helps organize and prioritize the work into a cohesive plan. Support for opioid stewardship must span the entire organization; an interdisciplinary approach is critical to gain fresh perspectives on your project and how it fits with your business strategy.
- Project management. Setting the appropriate scope, schedule and budget improves your chances of achieving desired results. Efficient use of management tools ensures effective use of time and encourages forward momentum.
- Information technology. This perspective is essential to provide insight into current capabilities and ease of data retrieval.
- Legal or compliance. Useful given ever-changing regulatory requirements.
- Patient advocates. They bring urgency to the work and convey critical but often unseen perspectives. Consider including representatives from Patient and Family Advisory Councils if available.”
In some rural healthcare settings, there may be fewer providers, staff, and/or resources. Many rural health teams have multiple commitments to existing committees related to other issues. One alternative to forming a large, new committee could be developing a small change team that reports out to, or is a sub-committee of, an existing committee (e.g., Medication Safety, Pharmacy & Therapeutics, Medical Staff Lead Committees, or even Quality Based/Patient Safety Committees).
(00:02:27)
Listen to Audio Clip
Why a rural Wisconsin health system developed two opioid stewardship task forces
Clip from Podcast with Sarah Pagenkopf, Director of Pharmacy Services, Fort Health Care
Listen to Podcast
Full Interview with Sarah Pagenkopf, Director of Pharmacy Services, and Tyler Prickette, Clinical Pharmacist at Fort HealthCare discussing:
- efforts to get buy-in from leadership to establish opioid stewardship task forces
- description of task force composition and reporting structure
- charter document guiding opioid stewardship and the task forces
- logistics of running the opioid stewardship task forces
- factors that contributed to success of task forces, and
- advice for pharmacist colleagues in rural settings
How do I go about forming an opioid stewardship leadership team?
The Society of Hospital Medicine (SHM) developed the Reducing Adverse Drug Events Related to Opioids (RADEO) Implementation Guide which provides step-by-step guidance to assist hospital teams in implementing a quality improvement program to improve patient safety and reduce opioid-related adverse events. The document provides detailed guidance for forming an interdisciplinary team, stating that to assemble such a team, it is important to identify the following:
Champion: This should be a well-respected individual (usually a provider) who is passionate about reducing opioid-related harms and who can promote the formation of opioid stewardship committee/task force and convey why it is important for your health system.
Executive-level allies: You will need support from the C-Suite or Executive level to ensure you have the resources and support to form the committee/task force. Often the Chief Medical or Nursing Officer take on this role and are actively involved in developing the charter and getting buy-in from administration and medical staff.
Leader: It is essential to have an individual who provides guidance and direction for the project. In some cases, this person may also be the champion, but this is not always the case. Importantly, this person needs to have dedicated time to spend on opioid stewardship.
Project Manager: If possible, it is ideal to have someone who has dedicated time to coordinate the day-to-day logistics of forming a committee (e.g., scheduling meetings, maintaining communication, compiling data, etc.).
In rural healthcare settings, where clinicians “wear many hats”, it is not uncommon for one person to be the champion, leader, and project manager.
A potential first step toward identifying a champion and allies who might have an interest in forming an opioid stewardship committee/task force, is to consider existing committees within your health system that would likely have an interest in, or be impacted by, opioid stewardship (e.g., Medication Safety, Pharmacy & Therapeutics, Medical Staff Lead Committees, or Quality Based/Patient Safety Committees). You might also consider providers in the organization, with strong opinions on pain management, patient experience, or a unique perspective on care delivery or opioids use.
Once you have identified potential committees or champions, you could request 5-10 minutes on the agenda of an already-scheduled committee meeting. Use that time to quickly and passionately present about the importance of opioid stewardship and be sure to include organizational data on opioid stewardship metrics, risks, or safety concerns at your health system.
This approach has several advantages in rural health systems, where providers and frontline staff often have multiple commitments to existing committees related to other issues: (1) it does not require an extra time commitment, as they had already planned to attend the meeting, and (2) pharmacy presence at these meetings will help to secure provider buy-in – as pharmacists are the “drug experts.” This might also be a method to obtain buy-in from the administration/leadership, especially if they attend this meeting as well.
This method of introducing opioid stewardship may have to be done repeatedly over time and across many committees, until you find the right fit. The second step is to identify providers or frontline staff who show an interest and passion in opioid stewardship. These individuals can be approached individually to assess their interest in being part of a separate sub-committee or committee/task focused on opioid stewardship.
Alternatively, you may be able to forego steps 1 and 2 if you can identify provider and staff colleagues who are passionate about opioid stewardship and would likely have an interest in joining a committee or task force. Module 3 has additional guidance on identifying champions for opioid stewardship who might be passionate about being part of an opioid stewardship committee/task force.
(00:03:25)
Listen to Audio Clip
How a pharmacy team at a rural Wisconsin health system got buy-in from leadership to initiate opioid stewardship task forces
Clip from Podcast with Sarah Pagenkopf, Director of Pharmacy Services, Fort Health Care
00:34:00
Listen to Podcast
Full Interview with Sarah Pagenkopf, Director of Pharmacy Services, and Tyler Prickette, Clinical Pharmacist at Fort HealthCare discussing:
- efforts to get buy-in from leadership to establish opioid stewardship task forces
- description of task force composition and reporting structure
- charter document guiding opioid stewardship and the task forces
- logistics of running the opioid stewardship task forces
- factors that contributed to success of task forces, and
- advice for pharmacist colleagues in rural settings
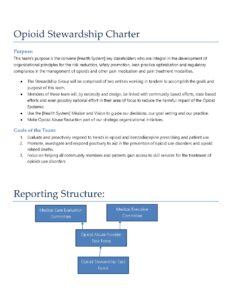
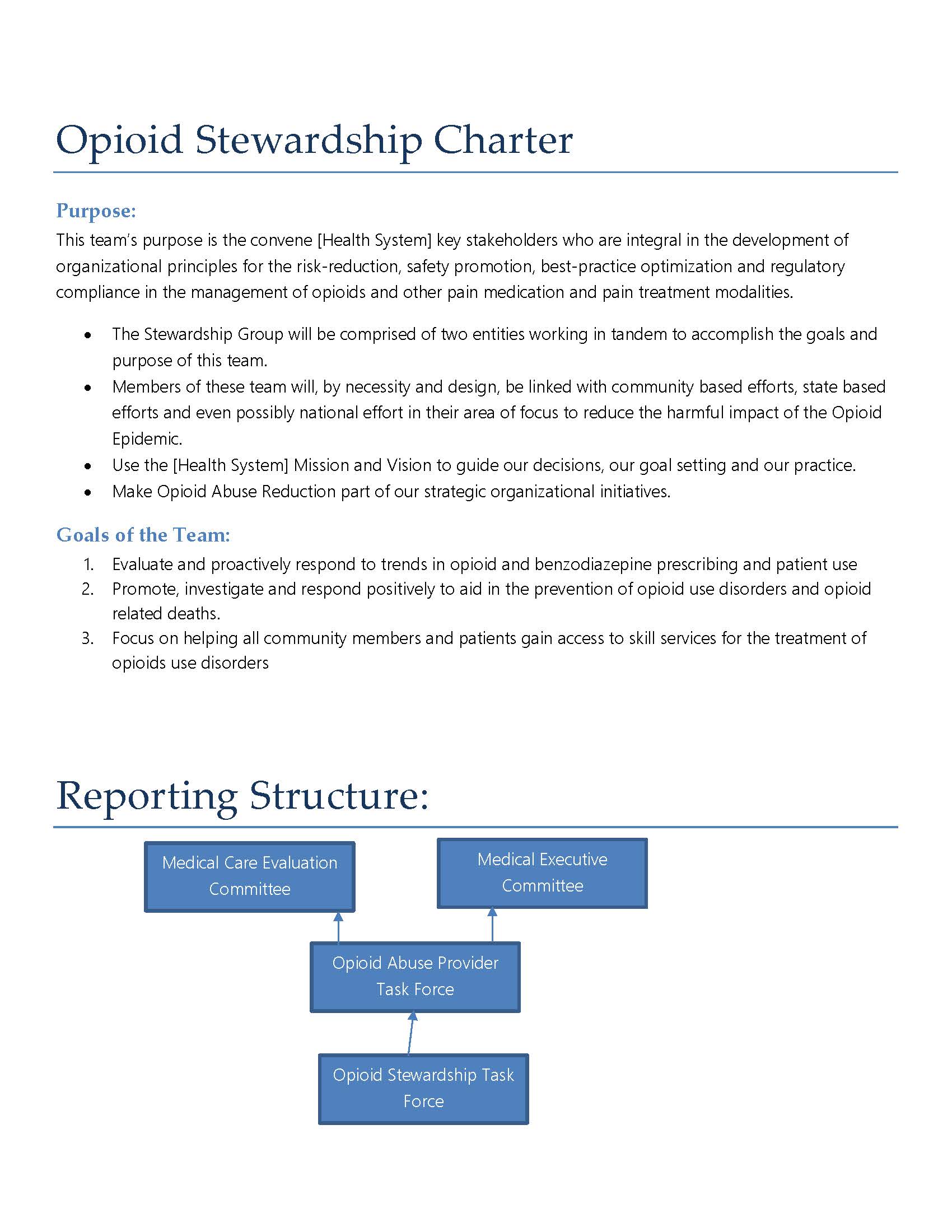 Another useful strategy to help the organization understand the need for opioid stewardship is to begin drafting a charter for the proposed opioid stewardship initiative. This document defines the purpose of the committee/task force, lists the goals of the team and often details the reporting structure for committee decisions/proposals. It lists the members who have committed to participate and provides a definition of the scope of the committee/task force. Preparing a draft of this document to circulate among prospective members and committees provides them with the details of the team’s vision for the committee/task force. The charter can be discussed and finalized during the first several meetings of the new opioid stewardship team or sub-committee.
Another useful strategy to help the organization understand the need for opioid stewardship is to begin drafting a charter for the proposed opioid stewardship initiative. This document defines the purpose of the committee/task force, lists the goals of the team and often details the reporting structure for committee decisions/proposals. It lists the members who have committed to participate and provides a definition of the scope of the committee/task force. Preparing a draft of this document to circulate among prospective members and committees provides them with the details of the team’s vision for the committee/task force. The charter can be discussed and finalized during the first several meetings of the new opioid stewardship team or sub-committee.
Who should be on the opioid stewardship leadership team?
A key characteristic of successful opioid stewardship committees/task forces is that they are multidisciplinary. It is important that the membership represents multiple layers of the organization and that it includes expertise from leadership, frontline clinical staff and relevant subject matter expertise. It is also crucial that those involved have sufficient influence within the organization that they can lead the efforts and will be supported at the highest level. (Society of Hospital Medicine, 2015)
Table 1. lists examples of disciplines typically represented on opioid stewardship committees/task forces. However, the specific disciplines represented depends on the goals and scope of your health system’s opioid stewardship initiatives. Some disciplines may be considered ad hoc, or as needed, members, depending on the specific goals and projects of the committee/task force.
Some key elements of committees/task force membership are:
- Support from Executive Leadership/Administration
- Leadership or involvement from Pharmacy
- Involvement of Information Technology/Systems
| Table 1. Examples of disciplines represented on opioid stewardship committees/ task forces | |
|---|---|
| Addiction Medicine | Nursing |
| Administration (e.g., Chief Medical Officer, Chief Quality Officer, Chief Information Officer) |
Pain Management |
| Anesthesiology | Patient education/advocacy^ |
| Behavioral Health/Psychiatry | Pediatrics |
| Billing/Business^ | Pharmacy |
| Community health liaison^ | Primary Care |
| Emergency Department | Physical/Occupational therapy |
| Family Medicine | Quality and Safety |
| Healthcare education | Social work |
| Information Technology/Systems^ | Supply Chain^ |
| Internal Medicine | Surgery |
| Legal/Compliance^ | |
^ = Ad Hoc or as needed
Table 2 provides details of a very inclusive membership list for an Opioid Stewardship task force. Your team, your goals, and your culture may require the inclusion of other members, or may not include some of these members/positions. As a team evolves, some of the members may not be needed or may be ad hoc and attend only on an as needed basis based upon specific goals or topics of the meeting. For example, a Prescription Drug Monitoring Program (PDMP) integration initiative might require input from IT, but other goals that do not include IT membership might not require IT attendance. Each rural health system should consider what the ideal membership would be for a task force or committee. However, do not be discouraged if you are not able to initially engage all individuals on your wish list. It is still possible to accomplish a lot with regard to opioid stewardship with a small and nimble team.
| Table 2. Planned Multidisciplinary Membership on Opioid Stewardship Task Forces | |
| Opioid Abuse Providers Task Force | Opioid Stewardship Task Force (Frontline) |
|---|---|
| Physician Chair | Co-Facilitator, Quality Director |
| Physician Member – ENT | Co-Facilitator, Pharmacy Director^ |
| Physician Member – Emergency Services | Advanced Practice Member – Hospitalists Group |
| Physician Member – Pain Management | Certified Nurse Anesthetists – Perioperative Services |
| Physician Member – Surgery | Pharmacy Clinical Specialist |
| Physician Member – OB/GYN | Ambulatory Pharmacist |
| Physician Member – Hospitalists | Emergency Services Director |
| Physician Member – Family Practice | Perioperative Services Manager |
| Physician Member – Pediatrics | Inpatient Services Manager |
| Advanced Practice Member – Family Practice | Inpatient Services Coordinator – Ortho Liaison |
| Physician Assistant Member – Family Practice | Education Services |
| Physical Rehabilitation Services Director | Behavioral Health Manager |
| Advanced Practice Member – Certified Nurse Anesthetists | Physical Therapy (inpatient and outpatient) |
| Chief Medical Information Officer | Nursery/GYN/OB Services Manager |
| Director of Information Technology Works | Pharmacy Clinical Specialist |
| Information Technology resource pharmacy | Lab team |
| Pharmacy Division staff | Health System Medical Group Clinic Manager |
| Senior Director – Admin member | Quality Analyst |
| Executive Director – Admin | Information Technology Works Analyst |
| Health System President & CEO | |
^ = members who are on both task forces
(00:02:18)
Listen to Audio Clip
Description of opioid stewardship task forces at a rural Wisconsin health system
Clip from Podcast with Tyler Prickette, Clinical Pharmacist, Fort Health Care
Listen to Podcast
Full Interview with Sarah Pagenkopf, Director of Pharmacy Services, and Tyler Prickette, Clinical Pharmacist at Fort HealthCare discussing:
- efforts to get buy-in from leadership to establish opioid stewardship task forces
- description of task force composition and reporting structure
- charter document guiding opioid stewardship and the task forces
- logistics of running the opioid stewardship task forces
- factors that contributed to success of task forces, and
- advice for pharmacist colleagues in rural settings
How should the opioid stewardship leadership team define their objectives, goals, and expectations of members?
Drafting a Charter
The team developing the opioid stewardship committee/task force should begin drafting a charter for the proposed opioid stewardship committee or task force. A charter is a document that outlines the goals and scope of the committee/task force. In creating an initial draft of the charter, the team can propose their vision for the purpose of the committee/task force, draft the goals of the team, and suggest a reporting structure for committee decisions and proposals. The draft charter document can then be circulated among potential committee/task force members to give them an idea of the proposed organizational vision for the committee/task force.
The charter can be discussed in the first several meetings. It can serve as a tool to guide the process of collaboratively defining the parameters for the committee/task force. Charters also typically list the members who have committed to participate and provides a definition of the scope of the committee/task force.
Download Example Opioid Stewardship Charter (PDF)
(00:03:31)
Listen to Audio Clip
Description of an opioid stewardship charter document from a rural Wisconsin health system
Clip from Podcast with Sarah Pagenkopf, Director of Pharmacy Services, Fort Health Care
Listen to Podcast
Full Interview with Sarah Pagenkopf, Director of Pharmacy Services, and Tyler Prickette, Clinical Pharmacist at Fort HealthCare discussing:
- efforts to get buy-in from leadership to establish opioid stewardship task forces
- description of task force composition and reporting structure
- charter document guiding opioid stewardship and the task forces
- logistics of running the opioid stewardship task forces
- factors that contributed to success of task forces, and
- advice for pharmacist colleagues in rural areas settings
Setting Goals
The goals defined by the opioid stewardship committee/task force will evolve over time and should be continually revisited and revised. It is important to document the goals agreed upon by committee members.
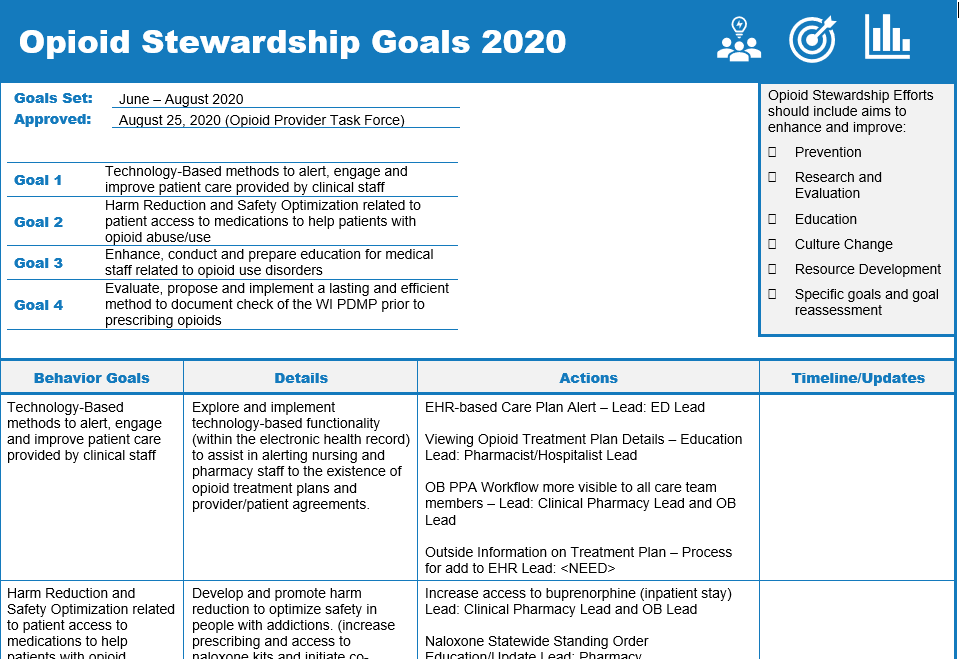 A team is most effective when the members are united under common goals. The Charter outlines team-based goals, and each year the team may consider more specific goals that align with the overarching team goals. Teams should be engaged to select goals that are specific, measurable, achievable, relevant to the larger goals of the team, and time-bound (SMART). Outlining annual goals is a productive way to unite the team under a common plan, visualize the goals for the coming year, and offers an opportunity to return to annual goals at each meeting, to check on progress, allow team members to provide updates, and to show action and results. This can facilitate building team morale and cohesiveness. Fort Healthcare provided a template used by their teams to outline annual goals.
A team is most effective when the members are united under common goals. The Charter outlines team-based goals, and each year the team may consider more specific goals that align with the overarching team goals. Teams should be engaged to select goals that are specific, measurable, achievable, relevant to the larger goals of the team, and time-bound (SMART). Outlining annual goals is a productive way to unite the team under a common plan, visualize the goals for the coming year, and offers an opportunity to return to annual goals at each meeting, to check on progress, allow team members to provide updates, and to show action and results. This can facilitate building team morale and cohesiveness. Fort Healthcare provided a template used by their teams to outline annual goals.
Module 3 provides further guidance about opioid stewardship goal setting.
Once an opioid stewardship leadership team is formed, how should we structure our meetings?
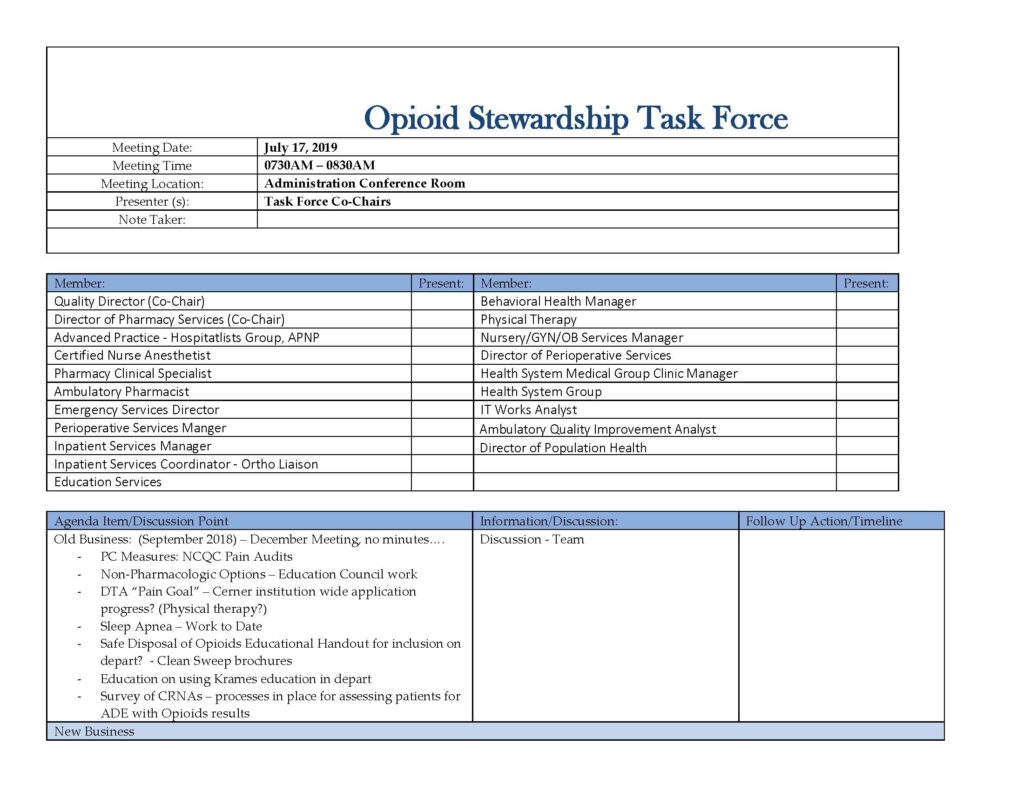 Teams are most effective when meetings are a good combination of information sharing, driving action, and reporting data. To engage your team, ensure that data, slides, materials and a clear agenda are provided in advance of the meeting (several days, up to one week before the meeting is a good practice).
Teams are most effective when meetings are a good combination of information sharing, driving action, and reporting data. To engage your team, ensure that data, slides, materials and a clear agenda are provided in advance of the meeting (several days, up to one week before the meeting is a good practice).
Download Example Opioid Stewardship Task Force Agenda (PDF)
Providing a clear agenda and summarizing the goals of the meeting helps increase attendance, shows actionable planning and helps attendees determine what to prepare. Meeting facilitators should consider any open action items from the previous meeting and alert attendees that were set to report on those topics, to ensure that they are ready to present. These reminders and facilitation keep the meetings action-oriented and goal-focused.
Be sure to consider the timing of the meeting, both at the time of the day and the duration of the meeting. Consider the schedules of attendees, when does patient care occur, when do the team-members have more time or options to meet and stay focused. Some rural organizations may find that providers are free before they see patients in their practice, and scheduling meetings very early may be helpful, others may find that providers or team-members prefer to meet over a lunch and make the meeting a working lunch meeting. Consider allowing a virtual meeting option. Virtual meetings allow providers/clinicians to log in from their office or desk and reduce travel time, which can help ensure ongoing participation. Also be sure to consider how long the meeting is scheduled to occur. The facilitator should take care not to overfill the agenda, only cover what you have time to cover – be thoughtful of the team members’ time, and don’t run late.
Finally, it is important to take notes that summarize the meeting discussion and follow-up actions. This is key to keeping the team on task and being action-oriented. Taking a few minutes at the end of each meeting to review the key points, or actionable items/homework to complete before the next meeting can be very helpful for the entire team. Facilitators can consider emailing or calling members that were assigned specific action items, and the facilitator should remember to add those items as ‘old business’ to the next meeting agenda.
(00:03:05)
Listen to Audio Clip
Logistics of managing opioid stewardship task forces at a rural Wisconsin health system
Clip from Podcast with Tyler Prickette, Clinical Pharmacist, Fort Health Care
Listen to Podcast
Full Interview with Sarah Pagenkopf, Director of Pharmacy Services, and Tyler Prickette, Clinical Pharmacist at Fort HealthCare discussing:
- efforts to get buy-in from leadership to establish opioid stewardship task forces
- description of task force composition and reporting structure
- charter document guiding opioid stewardship and the task forces
- logistics of running the opioid stewardship task forces
- factors that contributed to success of task forces, and
- advice for pharmacist colleagues in rural settings
What is an example of an opioid stewardship leadership team in a rural Wisconsin health system?
Listen to a podcast episode detailing an example of how a rural Wisconsin health system formed two opioid stewardship task forces.
Forming opioid stewardship task forces in a rural Wisconsin health system

Description:
- Interview with Sarah Pagenkopf, Director of Pharmacy Services, and Tyler Prickette, Clinical Pharmacist at Fort HealthCare discussing:
- efforts to get buy-in from leadership to initiate opioid stewardship task forces
- description of task force composition and reporting structure
- charter document guiding opioid stewardship task forces
- logistics of running the opioid stewardship task forces
- factors that contributed to success of task forces, and
- advice for pharmacist colleagues in rural settings
Where can I find additional guidance about forming leadership teams?
Two noteworthy resources provide detailed guidance about the formation of an opioid stewardship team.
- The College of HealthCare Information Management Executives (CHIME) put together an Opioid Playbook which has a chapter on Creating an Opioid Stewardship Committee. This chapter offers useful background information, general guidance on forming OS committee/task force and provides real world examples of committee development at health systems across the country, include a Wisconsin-based example from Gundersen Health System.
- The Society of Hospital Medicine (SHM) developed the Reducing Adverse Drug Events Related to Opioids (RADEO) Implementation Guide which provides step-by-step guidance to assist hospital teams in implementing a quality improvement program to improve patient safety and reduce opioid-related adverse events for patients receiving opioids. Pages 7-9 discuss the formation of an interdisciplinary team with a common goal and details how to assemble a team, establish team rules, and a charter.