The Centers for Disease Control identifies methicillin-resistant S. aureus (MRSA) as a serious health threat with greater than 100,000 invasive infections and 20,000 patient deaths annually in the United States. Despite recent advancements in available treatment options for methicillin-sensitive S. aureus and MRSA bacteremia, the morbidity and mortality attributed to this disease remains high. Significant gaps persist in our understanding of the progression of S. aureus infection and predicting patient response to treatment. Aggressive antimicrobial management is known to improve patient outcomes with S. aureus bacteremia, but current non-specific inflammatory markers fail to segregate high-risk patients for such therapies.
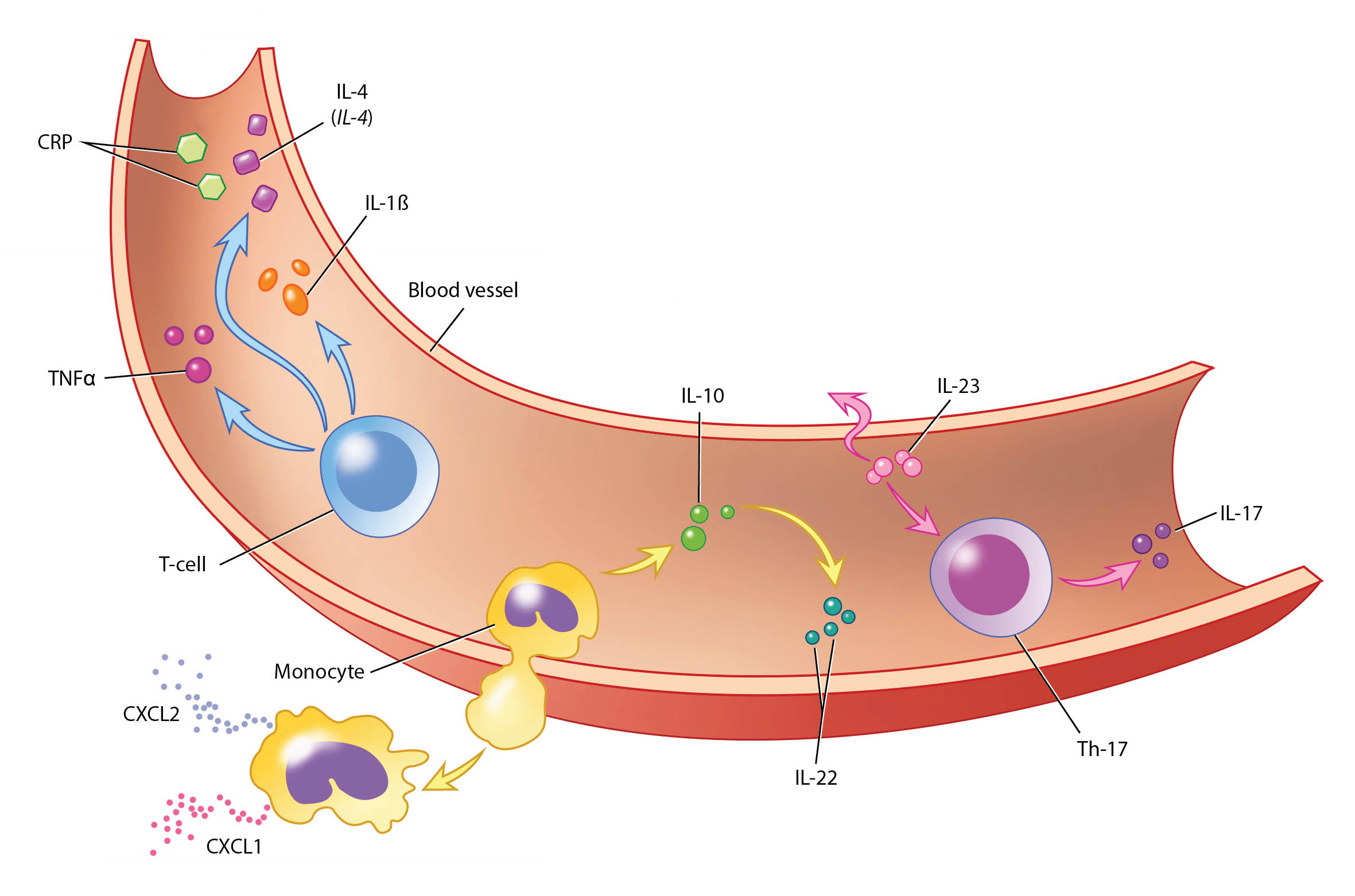
Over the past few years, we have collected a biobank of samples from patients with bacteremia at UW Health to understand the host-pathogen response in S. aureus bacteremia in order to better direct antimicrobial selection. This S. aureus Bacteremia and Immune Response (SaBIR) study has lead to a better understanding of the inflammatory to anti-inflammatory balance at the onset of serious infection. The innate host inflammatory response to S. aureus colonization and infection is extremely complex (see Fig. 3). However, using a targeted approach, we have identified cytokines as key predictors of patient mortality and persistent infection. In addition, patient genetics also appear to play an important role in bacterial clearance. We collaborate with investigators at the Marshfield Clinic and the University of California-San Diego to investigate these key metrics. This cross disciplinary collaboration has investigated new antimicrobial combinations in patients that can be used in these high risk patients to improve response. We anticipate these SaBIR studies will inform innate host biomarkers to direct a precision treatment approach with critical antibiotics and possibly non-antibiotics to patients most in need.

