
Nationally recognized for effective teaching and quality career preparation, the skills lab offers hands-on training based on best practices
By Katie Ginder-Vogel
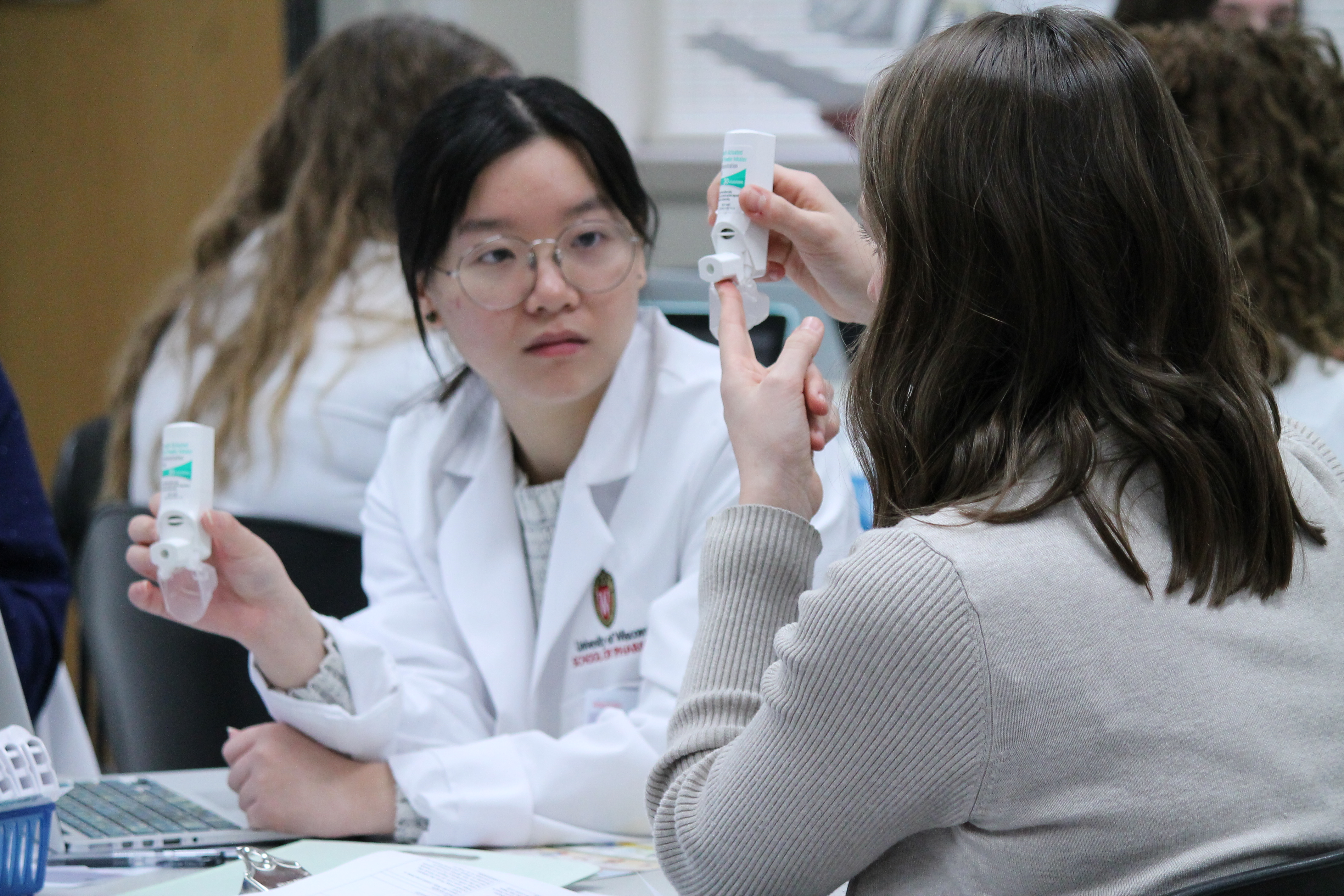
If asthma patients use their inhalers improperly — as research shows up to 90 percent do — they could be getting as little at 7 percent of the medication to their lungs, where it’s needed to reduce inflammation and open up restricted airways.
“Pharmacists are seeing asthma patients at every refill and can and should be a great resource to patients struggling to control their asthma,” says Susie Barnett (PharmD ’04), associate professor in the University of Wisconsin–Madison School of Pharmacy’s Pharmacy Practice Division. “We want our student pharmacists to get hands-on experience with these devices, so they can have meaningful and impactful conversations with their future patients, who might not even realize that they’re using their inhaler incorrectly.”
Alongside Associate Professor Andrea Porter (PharmD ’06), Associate Professor Casey Gallimore (PharmD ’05, MS ’13), and Assistant Professor Ed Portillo (PharmD ’14), Barnett is one of co-teachers for the School’s innovative and award-winning Integrated Pharmacotherapy Skills series, which gives PharmD students hands-on longitudinal and progressive training with patient consultation and education; documentation; and assessment of drug-related problems; as well as disease states including, but not limited to, asthma, diabetes, hypertension, and depression.
Our shared vision has allowed us to create something unique to Wisconsin that prepares students for a broad array of career paths.
—Ed Portillo
“Our goal is to teach students in the PharmD program the hands-on skills they’ll need and use as pharmacists — critical thinking and how to communicate with patients and providers,” explains Barnett.
The instructors use an evidence-based approach to assessing, designing, and improving course activities, with regular meetings to ensure students are developing the skill set necessary to contribute to patient care in a meaningful way. This iterative strategy has earned numerous national accolades, including the 2017 Rufus A. Lyman award and the 2018 Laboratory Innovations and Teaching (LITE) Award from the American Association of Colleges of Pharmacy (AACP), and serves as an example to pharmacy schools nationwide.
“Out of all the things we do, I’m proudest of our collective commitment to innovations in teaching,” says Gallimore. “We are continually striving to improve the learning experience for our students, and to improve our skills as educators.”
“Our shared vision has allowed us to create something unique to Wisconsin that prepares students for a broad array of career paths,” says Portillo.
Layered and progressive learning
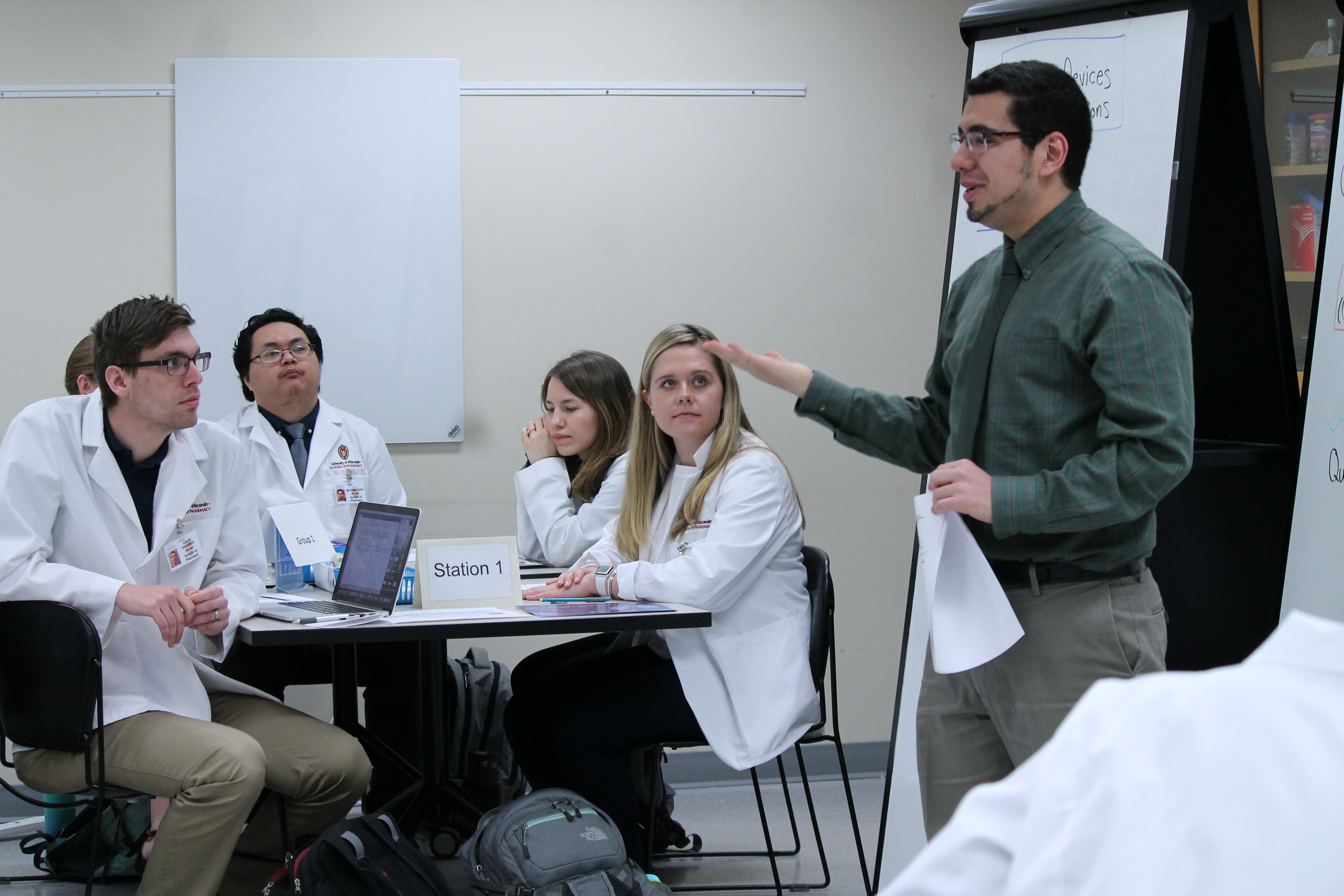
The two-year Integrated Pharmacotherapy Skills series begins with basic topics and skills, like how to take a medication history from a patient or a caregiver, and moves on to how to provide a patient consultation and administer injections, covering the skills pharmacists need with increasing complexity. The instructors design realistic simulations, similar to what students will see in practice.
“We all collaborate on the overarching structure and progression of the course sequence, to ensure the skills we cover progress appropriately in complexity and depth across all four semesters of the lab curriculum,” says Gallimore.
The instructors map out the skills students need to know and create lessons that build skills longitudinally over two years.
“We’ve undertaken extensive mapping exercises to envision which skills we are covering in which section of the course, how they’re assessed, the mechanism for feedback to students, and how they progress in complexity across the lab curriculum,” says Gallimore. “This mapping process was shared out as a model with other institutions in the form of both a manuscript and national webinar.”
Students practice each skill with peers or pharmacy residents, completing smaller graded activities before their big graded exams, which are hands-on and assess students’ skills.
“During the diabetes section, we acted as the patient in a diabetes foot exam and got hands-on experience in preparing and injecting insulin,” says third-year PharmD student Amanda Bernarde. “In the asthma/COPD section, we were given inhalers to prepare and test out. Both of these labs really put us in our patient’s shoes and allowed us to come up with potential issues with the medications.”
To teach documentation, which requires students to record patient interactions on the patient’s chart or in a conversation with a health provider, the instructors designed a three-lecture workshop series on writing. As part of that workshop, instructors showed students a video of a case, brought in pharmacists to talk about the different ways they handle documentation, and then had students share their thoughts.
“If you want to practice in an inpatient, clinic, or community pharmacy setting, you need this skill, and it’s technical and hard to do efficiently and effectively,” says Portillo.
The communication section of the Integrated Pharmacotherapy Skills series, much like the School’s Communication Skills Lab, also leverages standardized patients, who are community members employed by the Clinical Teaching and Assessment Center in the UW–Madison School of Medicine and Public Health. Standardized patients help student pharmacists practice interacting with real patients by teaching them how to use an inhaler or blood pressure monitor and performing simulated comprehensive medication reviews and annual wellness visits, both of which are services that pharmacists perform and bill for as part of the health care team in clinical settings.
The therapy lab curriculum equips students with a wide range of skills, enabling them to approach rotations with greater confidence in their ability to effectively perform as part of the health care team.
—Nick Friedlander
Third-year PharmD student Nick Friedlander values his experiences with standardized patients.
“It makes the whole experience feel real, like you’re interacting with a patient in a clinic trying to improve their health, rather than sitting across from someone trying to earn a good grade,” he says. “The simulated patients humanize pharmacy, and I think that’s essential when educating those who are responsible for improving the lives of others through good medical practice.”
Pharmacy residents and fourth-year pharmacy students on their Advanced Pharmacy Practice Experience (APPE) rotations join the instructors to help teach, assist with lab activities, lead case discussions, evaluate students, and provide feedback. Because residents have earned their PharmD degree just a year or two earlier, they are a valuable and relatable resource who can share real-world examples with students. With 35 to 45 pharmacy residents rotating through the skills labs each year, students meet residents from schools and pharmacies around the country.
“Lab-based courses need a lot of individuals to facilitate these types of performance-based activities,” says Porter, who is also the elected chair of AACP’s Laboratory Instructors Special Interest Group. “Faculty can’t do it all in courses like these. Bringing in residents and older PharmD students, including some third-year students taking an academic teaching elective, provides layered learning opportunities.”
Portillo says there’s a national discussion in pharmacy education about how to prepare pharmacy students for their final year of APPEs, when they’re out of the classroom and responsible for patient care in practice settings.
“We bring those outside experiences — clinic, hospital, community pharmacy — into the classroom,” says Portillo. “We provide a safe, collaborative environment, in which students learn from each other and receive timely feedback from instructors and residents. Not every school does that.”
“The skills I learned throughout the course were very practical,” says fourth-year student Zach Pedretti. “Lab prepared me to quickly assimilate and integrate myself into the health care team at the onset of my APPEs.”
Portillo regards his team as trailblazers at the forefront of situated learning, combining the content students are learning with simulations and having them repeat skills multiple times so they can see how the skill interplays with the content they learn.
“We have a very unique program, and the way we work together is really cohesive and beneficial, ensuring consistency in teaching across the four semesters of the course,” says Barnett.
National recognition for innovation and quality
The Integrated Pharmacotherapy Skills course is constantly changing, based on the latest skills students need to practice and feedback from fourth-year students and preceptors.
“One aspect of the course that is always adapting is the opportunity to practice teaching patients how to use different medication devices, such as inhalers, tobacco cessation products, or injections,” says Katie Flesch (DPH-3). “Between my second and third years, a new injectable migraine medication came on the market, and by the time classes started in fall, the lab already had samples of this injector, so that the second-year students could learn and practice the injection technique, in order to become comfortable teaching it to patients.”
That continuous quality improvement is what makes the UW–Madison School of Pharmacy’s course stand out on a national stage.

“We try to assess what we’re doing from multiple angles and sources, to determine if we’re achieving the desired educational outcomes that prepare our students for APPE rotations, while still providing a positive educational experience from the student perspective,” says Gallimore. “This included a step-wise assessment process several years ago, to completely revamp our lab curriculum. For this, we surveyed and held focus groups with preceptors from varying areas of practice and current students.”
That assessment earned Barnett, Gallimore, and Porter the 2017 Rufus A. Lyman award for the most impactful paper published in the American Journal of Pharmacy Education (AJPE) in 2016. Their manuscript describes the qualitative and quantitative assessment methods the instructors used to identify the existing skills labs’ strengths and weaknesses.
“The paper talks about how to evaluate the successes and challenges of a course series in a quantitative and qualitative way and how to re-tool the course accordingly,” explains Barnett. “It’s shone a light on the value of what the skills lab does for our curriculum, and that’s validating for us as well as lab faculty around the country.”
Individually and together, Barnett, Gallimore, Porter, and Portillo have published multiple manuscripts on the scholarship, teaching, and learning within the skills lab.
“I’m very proud of how collaborative our group is,” says Barnett. “We genuinely work well together and make a concerted effort every year to innovatively revise the activities and curriculum to better serve our PharmD students, and these awards demonstrate that. We feel so lucky to be working together.”
We are continually striving to improve the learning experience for our students, and to improve our skills and educators.
—Casey Gallimore
Barnett and Gallimore were awarded a 2019 University of Wisconsin Educational Innovations grant for a project aimed at improving the communication of pharmacy students through increased practice scenarios. Barnett won a University of Wisconsin Educational Innovations mini-grant in 2014 to understand the impact virtual patient cases have on student knowledge, which led to the development of additional virtual simulated patient cases in the lab series.
In July 2018, Barnett and Portillo received the Laboratory Innovations and Teaching Award (LITE) Award from AACP in 2018 for using video modeling to teach student pharmacists how to present a complex patient to a pharmacy preceptor.
“We received the LITE award for doing something we found simple and useful that made learning certain skills more accessible,” says Barnett. “I think the award shows how you can use limited resources to improve student learning and better use faculty and student time.”
Translating to practice
Friedlander, who is a teaching assistant for the Integrated Pharmacotherapy Skills course this year, is considering transplant pharmacy as a future career and says the lab has helped him develop and sharpen crucial competencies, such as drug-related problem identification, patient interviewing, provider communication, and clinical problem-solving.
“Given the complexity of the typical transplant patient, interprofessional communication and drug-related problem identification skills are invaluable in delivering patient-centered care,” says Friedlander. “The therapy lab curriculum equips students with a wide range of skills, enabling them to approach rotations with greater confidence in their ability to effectively perform as part of the health care team.”
As a pharmacy intern, Friedlander says he regularly leverages his patient consultation training.
“During my summer internship, I participated in several clinical pharmacy visits focused on hypertension management, during which I had to perform manual blood pressure checks,” he says. “Because of this skills lab, gathering blood pressure readings manually felt so natural to me by the time I performed it in my internship that it became one of my favorite summer experiences.”
During Bernarde’s rotations, she says she used the framework of counseling and patient case presentations she learned in the Integrated Pharmacotherapy Therapy Skills courses to prioritize drug problems and counseling points.
“Some patients may have more drug-related problems than what can be handled at that moment, at that visit, or on that day,” she says. “As a medical professional, it’s critical to be able to prioritize problems or counseling points, in order for the patient to receive the most benefit without overwhelming them with information or changes.”
“I hope students walk away from the course with a skill set that allows them to provide patient-centered, team-based care,” says Gallimore. “I also hope we’ve helped them to develop critical thinking and problem-solving skills that can be applied in addressing health-related problems, and allow them to contribute in a meaningful way as medication experts on health care teams.”
Learn about another innovative course in the UW–Madison School of Pharmacy’s PharmD curriculum: the Communications Lab.












