To combat the US opioid epidemic, massive efforts have been focused on expanding access to medications for opioid use disorder (MOUD). While there are indications of improved reach and adoption, an ironic gap persists—only about one-third of specialty addiction treatment organizations offer MOUD. This proposal, Stagewise Implementation-To-Target – Medications for Addiction Treatment (SITT-MAT) funded by the National Institute on Drug Abuse, not only advances the science of implementation, but advances our empirical understanding of how to best respond to a substance-related epidemic.
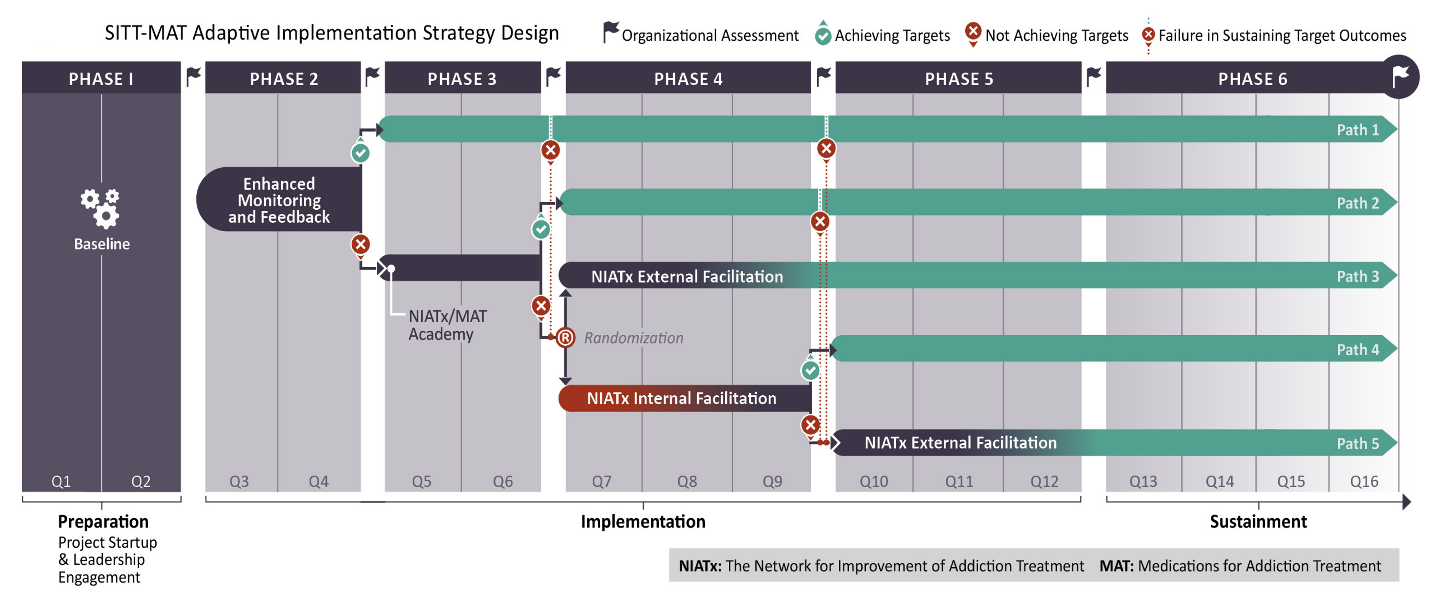
The SITT-MAT project continues our prior collaboration with Dr. Mark McGovern at Stanford University. Within an adaptive implementation strategy trial design, using an innovative stagewise implementation-to-target approach, approximately 60 community addiction treatment programs in the State of Washington will participate in the project. The stagewise implementation-to-target, stepped “care” type approach, deploys increasingly intensive strategies only if needed (see Figure).
Unprecedented funding has been allocated to combat the US opioid epidemic. Through the 21st Century Cures Act, over $5 billion has been directed to the Substance Abuse and Mental Health Services Administration (SAMHSA) and the National Institutes of Health’s Helping to End Addiction Long-term (HEAL) initiative.34–36 The mission has three parts: reduce opioid over-prescribing, improve access to overdose rescue medications, and increase the adoption and delivery of medications for opioid use disorder (MOUD).34,35
Efforts have been primarily focused on expanding access to MOUD. The SAMHSA State Targeted Response and the State Opioid Response grants to 57 US states and territories sought to expand access to methadone, buprenorphine and naltrexone across a variety of settings and systems.35,37 Through the HEAL initiative, significant research is addressing problems with access and retention by evaluating improved delivery platforms for addiction medications.36 For example, through two large RFAs, the National Institute on Drug Abuse (NIDA) launched substantial research to build community responses in highly impacted states, and stimulated multi-state campaigns to engage persons who are incarcerated or on probation or parole.38
While there are indications of improved access across a variety of settings, an ironic gap persists.16,39–43 Primary care practices, emergency departments, and the criminal justice system have increasingly adopted MOUD, but traditional specialty addiction treatment programs have not progressed. Currently, only 35.5% of addiction treatment programs offer MOUD.39 Sadly, only 15% of patients in specialty addiction treatment with OUD are receiving MOUD.16,17 In fact, general medical practice settings are now twice as likely to offer MOUD than are specialty addiction treatment programs.44–46
Specialty addiction treatment programs are under pressure to implement MOUD but face many barriers.40,43,47–50 Public health systems now support MOUD in policy and financing, but multiple contextual barriers persist, ranging from an abstinence-based philosophy that conflicts with pharmacological approaches, a lack of network connectivity with other health care organizations, and program structure and workflows based entirely on psychosocial interventions and peer recovery supports.51–53 Although there has been progress among some specialty programs, most lag behind.17
Implementation research is poised to address situations where proven treatments exist but are not widely available.54,55 Implementation research has progressed beyond theories, models, and frameworks.56 Designed to solve public health problems through the application of scientific methods and measures, implementation research is increasingly rigorous.57 Such methods are sorely needed when evidence-based interventions are not accessible to the people who need them the most–clearly the case for persons with OUD seeking help from those who ostensibly provide specialty addiction treatment services.58
Advances in the characterization of context, and in the evaluation of outcomes, demonstrate methodological progress for implementation science. The characterization and measurement of context, a determinant of successful or unsuccessful implementation, has made headway. Context can be organized by levels: the outer context (systems and community), inner context (the organization or setting), individuals (such as physicians and/or therapists), and perceptions of the intervention to be implemented.59,60 Measurement of implementation outcomes has also been refined. For example, the RE-AIM taxonomy is an acronym organized by Reach (numbers or proportion of eligible individuals receiving the intervention), Effectiveness (a measure of whether the intervention is working), Adoption (the number or proportion of individuals and/or sites delivering the intervention), Implementation (a measure of fidelity that the intervention is being delivered as designed), and Maintenance (a measure of the sustainment of the intervention over time).61,62
The science of implementation continues to enhance rigor by systematically examining implementation strategies as the “interventions” of implementation. In an elegant distinction by Curran, “interventions” are described as THE THING, and “implementation strategies” are described as how we get systems, organizations and practitioners to DO THE THING.63 This distinction is critical yet often confused by intervention developers, evaluators or trialists who install an intervention rather than study how to implement it. Further, an installation by research personnel and study physicians is altogether different than a routine implementation by existing staff in the real world and in the absence of time-limited research funding. More recently, experts have called for implementation strategies to be examined by: 1) their discrete and combined components; 2) conceptualized mechanisms of action; 3) how they may be tailored or adapted to context or other factors; 4) how they may be delivered with fidelity; 5) how enrolled participants engage and finish; 6) how alternative strategies compare with one another on implementation outcomes; and, 7) how much they cost. 57,64–66 Although exemplar studies featuring some of these expert recommendations for implementation strategies do exist, none to date feature all, and none are in the critical field of implementing MOUD
Specific Aim 1: Within a stepped measurement approach, that includes a randomized implementation trial, to evaluate the relative impact of a sequence of four implementation strategies on target outcome criteria: a) proportion of patients on addiction medication (buprenorphine or naltrexone) for opioid use disorder; b) number of onsite prescribers; c) proportion of patients receiving medication within 72 hours of diagnosis of opioid use disorder; and d) 6-month retention.
Specific Aim 2: To examine contextual moderators and mediators of performance on target outcomes as a function of implementation strategy step. Moderators include program characteristics, contextual factors, and baseline status. Mediators include program participation in strategies and fidelity to the implementation strategy model.
Specific Aim 3: To document the costs associated with participation in the sequence of implementation strategies, and to model costs per implementation strategy to achieve target outcome criteria.
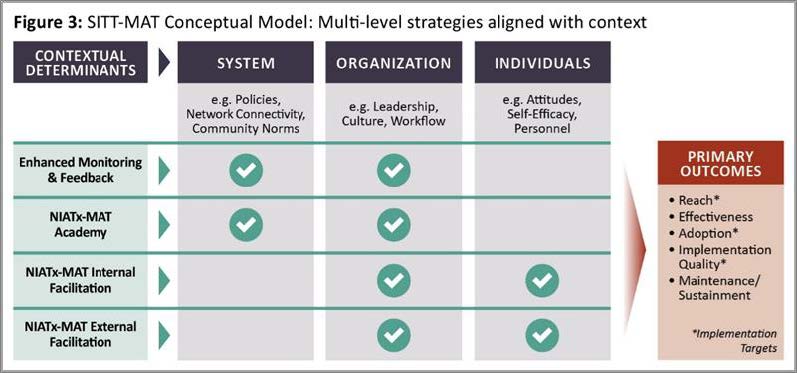
Influenced by thought leaders in dissemination and implementation science, our conceptual model is based upon matching implementation strategies to levels of contextual determinants, i.e. barriers or facilitators, to produce desired outcomes (see Figure).⁵⁹,⁶⁵,¹⁰⁷ Like any conceptual model, this process is not linear but dynamic. In implementation research, studies like ours provide actual data for downstream validation.
Contextual determinants may operate at 3 levels: systems, organization, and individuals. The Consolidated Framework for Implementation Research (CFIR) provides an inventory of barriers and facilitators within these levels.⁵⁹ System level factors include policy, community, and financial levers. In MOUD implementation by specialty addiction programs, system barriers include myths about prohibitive policies, historical isolation from other health care providers, and norms that do not endorse MOUD. Organization level barriers include leaders who may not support MOUD, a culture of anti-MOUD as “just another crutch” and inflexible daily schedules. At the Individual level, many of these barriers are manifest in one’s own personal experience with addiction recovery, the lack of physicians or any licensed prescriber, and addiction counselors’ fears about the “professionalization” of the field.
Implementation strategies might address potential barriers at each level in order to implement MOUD, but presently there are no solid empirical bases for selection and tailoring based on contextual determinants. ¹⁰⁸,¹⁰⁹ Instead we were guided by four criteria in our selection: 1) the evidence for each strategy: 2) the standard practice of using the strategy to address typical implementation problems at the determinant level; 3) our own research; and 4) the incremental effort and cost associated with each strategy.