This project will evaluate the impact of the Wisconsin UTI Improvement Toolkit on antibiotic prescribing for UTI and assess the influence of external facilitation on adoption and effects of the toolkit in Wisconsin NHs. The primary study objectives are to assess the overall impact on antibiotic utilization and determine the extent to which effects vary by the implementation approach employed. We will achieve these two objectives through the following specific aims: 1) Evaluate the impact of the Wisconsin UTI Improvement Toolkit on antibiotic prescribing for UTI in Wisconsin NHs and 2) Assess the influence of external facilitation on adoption and effects of the Wisconsin UTI Improvement Toolkit in Wisconsin NHs.
Overuse and misuse of antibiotics is a major public health problem in Wisconsin nursing homes (NHs) [1] that adversely impacts resident and community health through adverse drug reactions [2], Clostridium difficile infections [3] as well as development and spread of antibiotic-resistant bacteria [4,5].
Treatment of suspected urinary tract infection (UTI) accounts for nearly half of the antibiotic use in Wisconsin NHs [1]. Less than half of the antibiotics prescribed for UTI in Wisconsin NHs are not justified [6] and improving the management of UTI in NHs has been identified as a major priority by experts in the field [7-9].
We along with our community partners have developed a toolkit of evidence-based practices for improving the management of UTIs in Wisconsin NHs (hereafter referred to as the Wisconsin UTI Improvement Toolkit). While use of the practices incorporated in the Wisconsin UTI Improvement Toolkit has resulted in notable improvements in the quality of antibiotic prescribing for the treatment of UTI in a number of studies [10-12], more limited effects have been observed in other studies despite employing similar improvement strategies [13-15]. Heterogeneity of effects across different settings is a problem commonly encountered with healthcare behavioral interventions and may arise due to characteristics of the intervention, the setting into which it is being introduced and the method of implementing the intervention in that setting [16]. There are a number of challenges to improving quality in NHs, including lack of improvement expertise [17] and high levels of staff turnover [18] to name a few. It is unrealistic to expect that these structural barriers will abate anytime soon. Consequently, it is critically important to identify effective strategies to overcome them if meaningful improvements in the quality of antibiotic prescribing in NHs is to be achieved.
Specific Aim 1: Evaluate the impact of the Wisconsin UTI Improvement Toolkit on antibiotic prescribing for UTI in Wisconsin NHs.
Specific Aim 2: Assess the influence of external facilitation on adoption and effects of the Wisconsin UTI Improvement Toolkit in Wisconsin NHs.
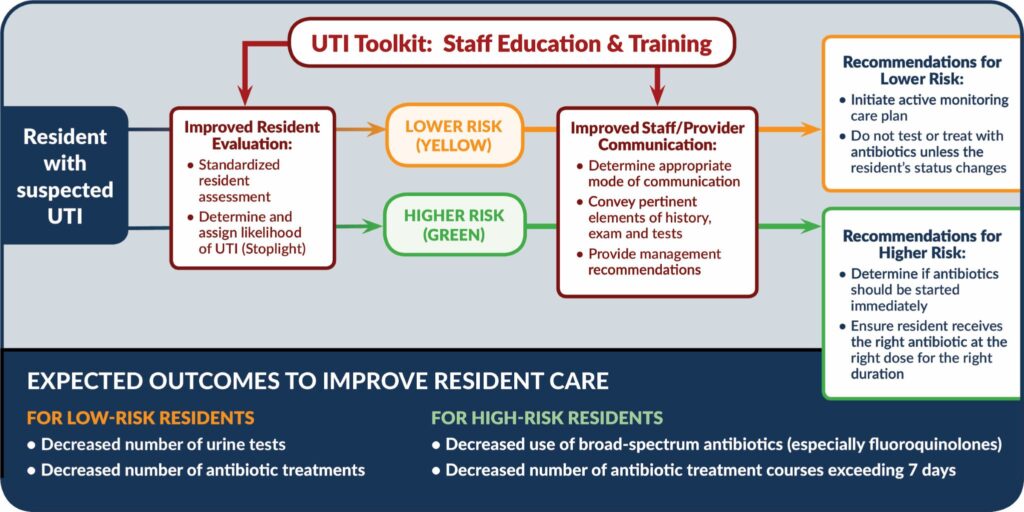
The behavioral objectives of the toolkit are to (1) improve nursing staff assessment of residents experiencing a change in condition potentially attributable to UTI; (2) improve the quality of inter-professional communication when a diagnosis of UTI is being considered; (3) ensure that nursing staff and clinicians ascertain the likelihood of UTI (low vs high probability); (4) defer urine testing and antibiotic therapy when the probability of UTI is low; and (5) prescribe antibiotics appropriately (choice of agent and treatment duration) when the probability of UTI is high.