Despite the implementation of health information technology (health IT) targeting medication safety, ambulatory adverse drug events (ADEs) prompt over four million people to seek medical care and result in $8 billion in health care expenditures annually. One critical gap that Health IT has not meaningfully addressed is the electronic communication of medication discontinuation orders between prescribers and community pharmacists in the outpatient setting.
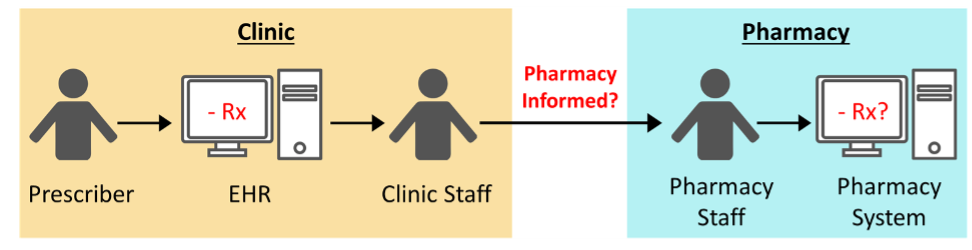
Prescribers routinely discontinue prescriptions electronically in the electronic health record (EHR) during outpatient clinic visits. Although these modifications are automatically documented in the EHR, medication discontinuation orders are not communicated to the patient’s pharmacy management software. Instead, such communication is a manual process, delegated to clinic staff who call or fax the pharmacy to notify them of the discontinuation.
Given the demands already placed on clinic staff, these orders are rarely communicated to the pharmacy. Thus, despite being removed from the EHR, discontinued medications remain on the community pharmacy list, resulting in medication list discrepancies.
Medication list discrepancies create a serious and alarming vulnerability that allows discontinued medications, even those discontinued due to a serious adverse drug reaction, to be repeatedly dispensed. Indeed, up to 5% of discontinued medications are later dispensed, with 34% of these events meeting the criteria for high risk for potential ADEs.
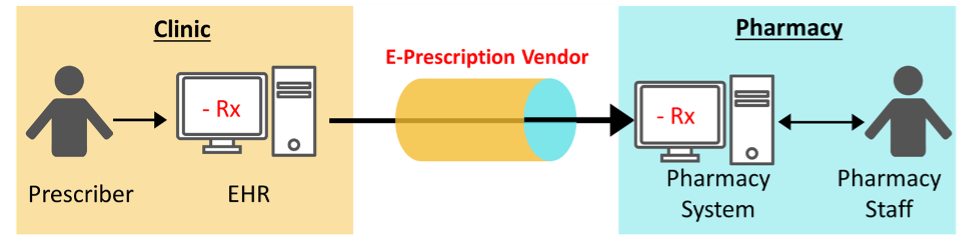
CancelRx is an e-prescribing transaction that communicates a medication discontinuation order between the EHR and pharmacy management software and has the potential to reduce medication discrepancies and thus improve medication safety.
The CancelRx research portfolio has been supported by multiple funding sources including the Gorden and Betty Moore Foundation (2017), Agency for Healthcare Research and Quality (2018), University of Wisconsin–Madison Office of the Vice Chancellor for Research and Graduate Education with funding from the Wisconsin Alumni Research Foundation (2018), the NCPDP Foundation (2019), and the by the Clinical and Translational Science Award (CTSA) program, through the NIH National Center for Advancing Translational Sciences (NCATS), grant UL1TR002373.