This study examines how CancelRx, an e-prescribing functionality that communicates medication discontinuation orders between the clinic and pharmacy, impacts the cancellation and dispensing of prescription medications.
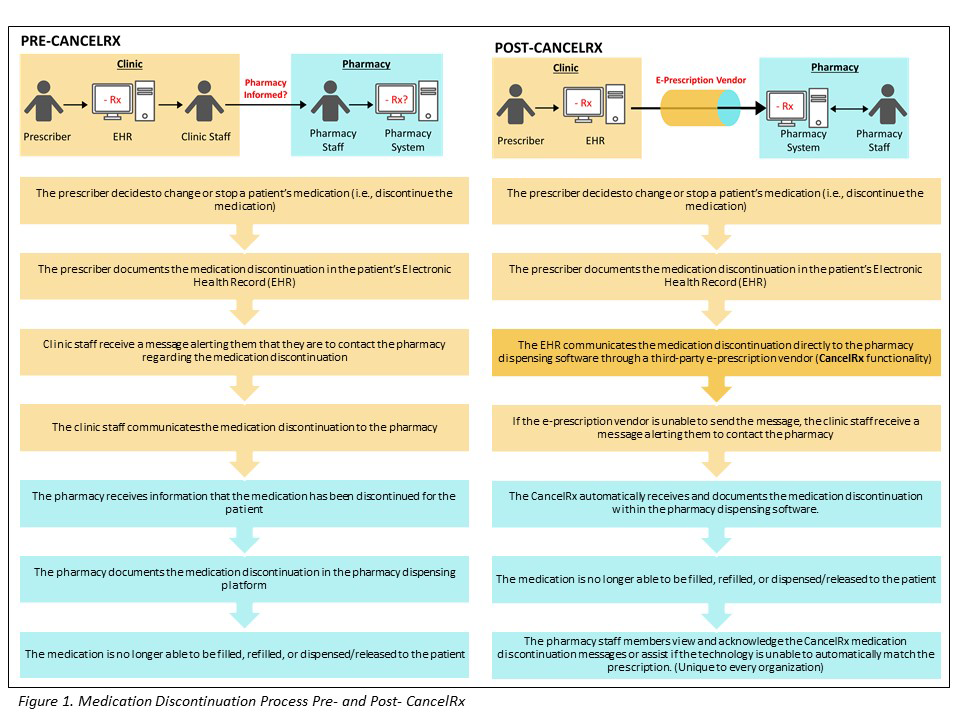
When a patient is seen in an outpatient clinic, the prescriber may discontinue medications. Although these changes are documented in the clinic electronic health record (EHR), there typically is no automatic transmission of this information to the pharmacy—creating discrepancies in the patients’ medication lists and making patients vulnerable to errors (e.g., dispensing medications that were stopped due to dose changes, drug changes, or even adverse events). A new health information technology (IT), CancelRx, recently was introduced to electronically send a medication cancellation message from the clinic to the pharmacy.
Aim 1. To measure the impact of CancelRx on reducing medication discrepancies in the pharmacy management software.
Aim 2. To describe the impact of CancelRx implementation on outpatient clinic and community pharmacy work systems.
UW Health is the integrated health system of the University of Wisconsin-Madison serving more than 600,000 patients each year in the Upper Midwest and beyond with 1,400 physicians and 16,500 staff at six hospitals and 80 outpatient sites. UW Health has 15 pharmacies
UW Health began implementing the Healthlink EHR (Epic Systems Inc., Verona, WI) system-wide in 2006. E-prescribing is currently the preferred route of prescribing at their outpatient clinics. UW Health clinicians e-prescribe over 1.5 million prescriptions annually.
UW Health community pharmacies implemented Enterprise Rx (McKesson, San Francisco, CA) in 2008. Enterprise is a pharmacy management software and is a different system than Healthlink EHR. Enterprise serves as the primary health IT tool to verify the accuracy and appropriateness of and dispense prescription medications in the community pharmacy. E-prescribing is currently the preferred route of receiving new or refilled prescriptions. UW Health Pharmacies fill approximately 500,000 prescriptions annually.
CancelRx was introduced as part of a larger health IT update in October of 2017 at UW Health Hospital and Clinics, with all prescribers gaining access to this functionality at the same time.
The conceptual model for this study is adapted from the Interactive Sociotechnical Analysis (ISTA) framework.
The ISTA framework is a conceptual model that uses a work system approach to understand how unintended consequences arise from the implementation of health IT. Its premise is that undesirable outcomes flow from the interplay between the new health IT and the work system. The work system is divided into two components: the health care organization’s existing technology (referred to as the technical system), and the health care organization’s existing workers, workflow, culture, tasks, and work processes, and social interactions (referred to as the social system). These interactions together are referred to as sociotechnical interactions. The ISTA framework recognizes that the “actual use” of the health IT must be examined, not just the health IT “as designed.” It also emphasizes the recursive nature in which the social system interacts with the health IT to mediate how it is used, which can then change the social system.
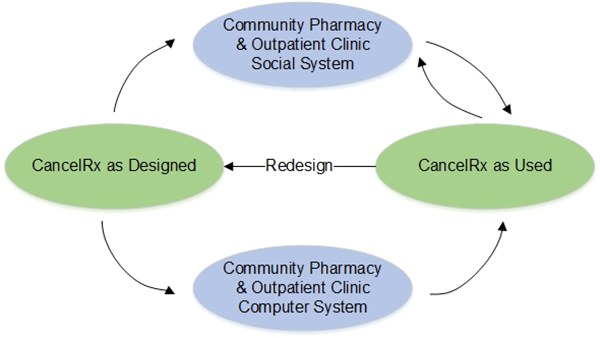
In Aim 1, we examined the effect of CancelRx on removing discontinued medications from the community pharmacy management software. A CancelRx transaction is generated and sent from the EHR when medications are electronically discontinued. Successful transmission requires that the community pharmacy management software allows for incoming CancelRx messages, allows for messages to be generated by the community pharmacy computer system back to the EHR, and provides an efficient way to deactivate the discontinued medications. Therefore, the design of community pharmacy management software mediates how CancelRx is operationalized in the community pharmacy.
In Aim 2, we identified how CancelRx implementation impacts both the outpatient clinic and the community pharmacy social systems (focusing on the people in the system, the tasks they perform, and the organizational culture). The clinic and pharmacy social systems interact with CancelRx as designed to affect how CancelRx is used. Because the ISTA framework emphasizes the recursive and iterative nature of these relationships, we collected data following CancelRx implementation to assess how the outpatient clinic and community pharmacy social systems shape CancelRx over time. We will focus on adoption and implementation at the 3-month data collection and maintenance at the 9-month data collection.
Aim 1 Data Sources, Data Collection, and Measures
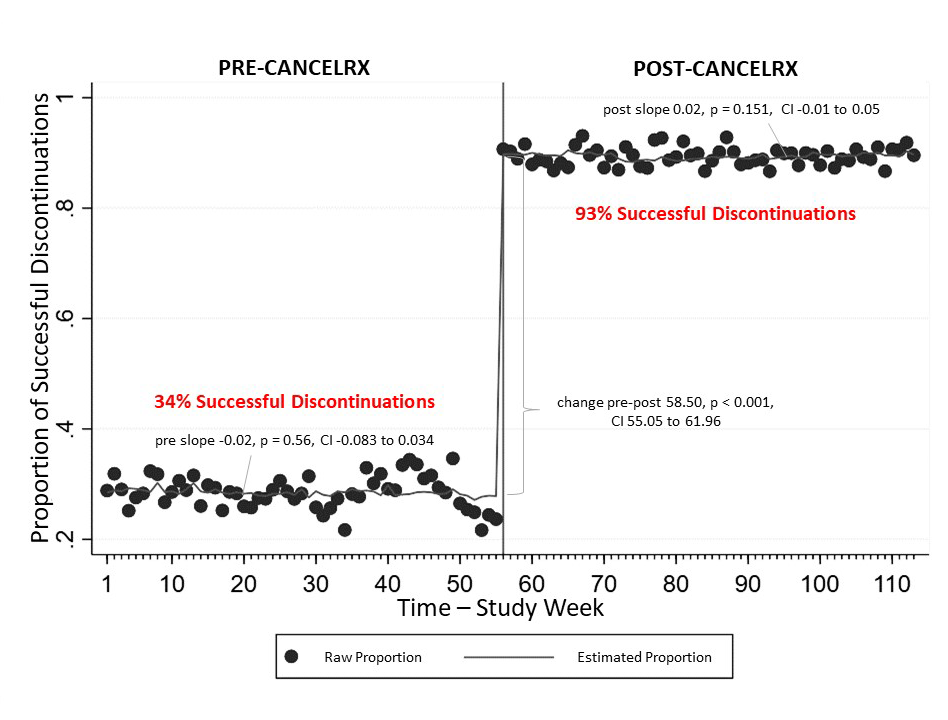
The research team used an interrupted time series analysis (ITSA), a longitudinal quasi-experimental design, to evaluate the effect of CancelRx to decrease medication discrepancies in the EHR and pharmacy management software.
Data collection took place during a 12-month pre-intervention and 12-month post-intervention period. Each measurement constituted one week in the time series. The post-intervention period started 4 weeks after CancelRx implementation, as an a priori burn-in period to allow for resolution of technical problems after CancelRx go-live.
Data were extracted and merged from the clinic EHR and pharmacy dispensing software using an e-prescription order ID when available. To account for instances when an e-prescription order ID did not exist, EHR and pharmacy dispensing data were matched on the following variables: patient gender, drug description (name, strength), ordering department, and a drug discontinuation time within a 72-hour window between the clinic and pharmacy systems. For this study, only cancellation messages in which a prescriber indicated that the pharmacy should be contacted were included in the analysis.
Interrupted Time Series Analysis (ITSA)
The research team conducted the ITSA to model the occurrence of “successful” discontinuations in which a medication that was discontinued in the clinic’s EHR was also discontinued in the pharmacy’s management system. For this study, “successful” discontinuation was one in which 1) discontinuation data matched 2) the medication was discontinued in EHR, and 3) the medication was discontinued in the pharmacy dispensing software within 72 hours. The team used Prais-Winsten estimation for the ITSA. The analysis was conducted in STATA.
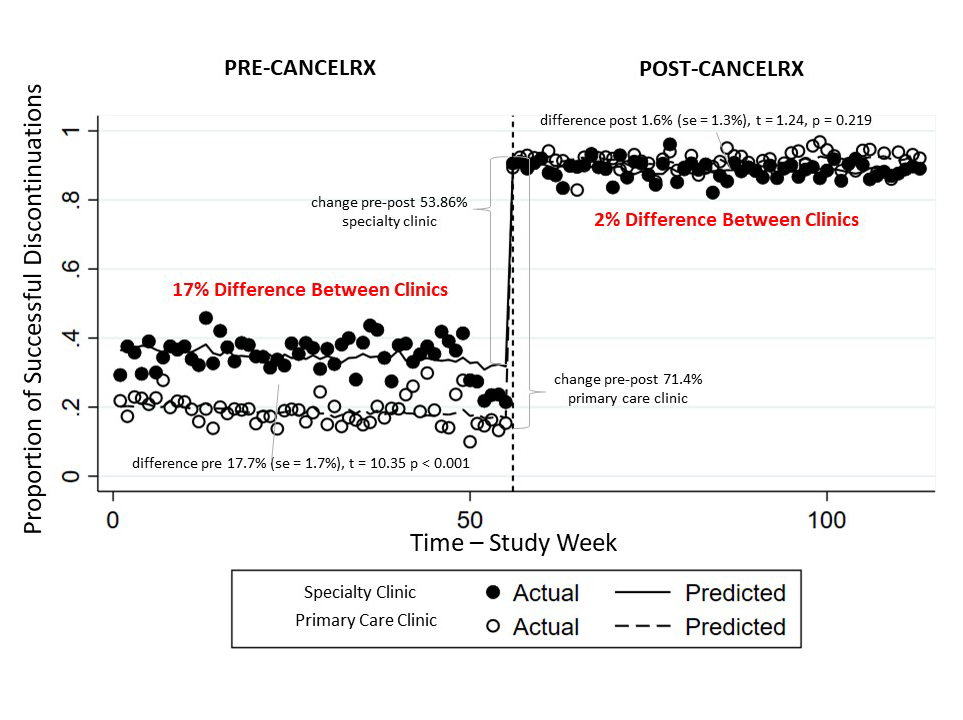
Sample Subsets
The research team also subset the data based on the type of clinic in which the cancellation message originated. A clinic was deemed as either primary care—consisting of internal medicine, family medicine, general pediatric, general geriatric or obstetrics/gynecology—or specialty practice (e.g. gastroenterology, cardiology, endocrinology, etc.).
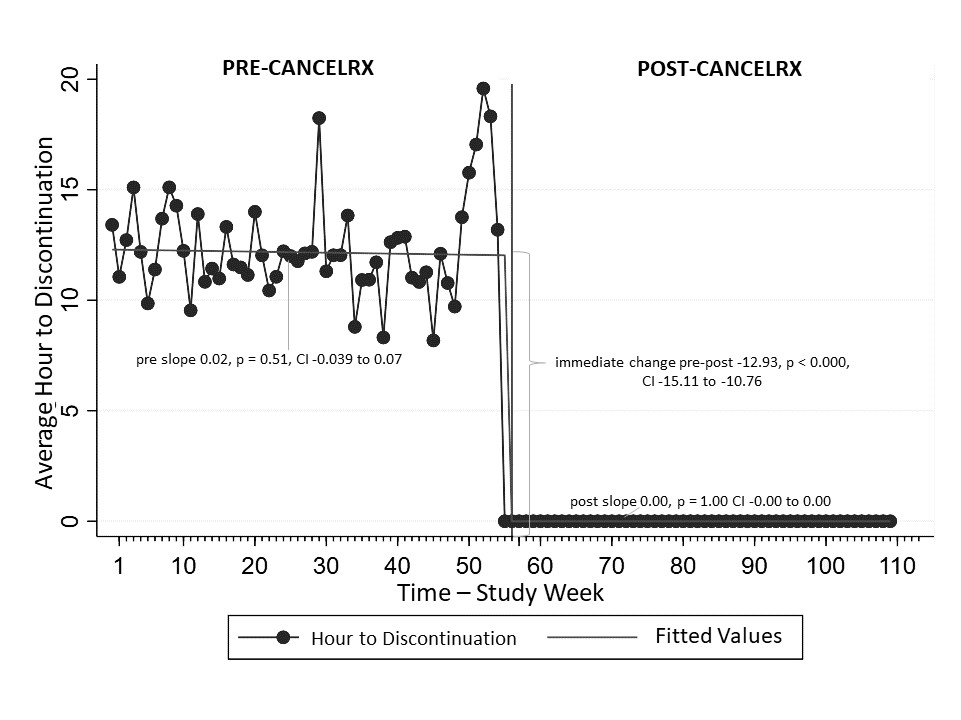
Time to Discontinuation
The research team conducted the time-to-discontinuation analysis by comparing the date of discontinuation in the EHR data to the pharmacy data. The time to discontinuation was aggregated and averaged for each week in the study period and compared over time using Regression with Newey-West standard errors.
Aim 2 Data Sources, Data Collection, and Measures
In order to understand the clinic and pharmacy work systems and how their characteristics facilitate and hinder implementation and use of CancelRx, data were collected at three-time points: pre-intervention, 3-months post-intervention, and 9-months post-intervention.
The focus on the pre-intervention data collection was to gather baseline information about current work processes, workflow, and workload. The focus of the 3-month post-intervention data collection was to understand adoption and implementation of CancelRx in the clinic and pharmacy work systems. The focus of the 9-month data collection was to understand how the work systems reshaped to facilitate maintenance of effective CancelRx use.
Medical Assistant Interviews
A total of 27 interviews with end-users were conducted (three interviews pre-intervention, three interviews 3-months, and three interviews 9-months post-intervention at each of 3 outpatient clinics).
Pharmacist/Technician Observations
The purpose of the observations was to gain insight into fit and compatibility of the intervention within the pharmacy work system. A total of 26 3-hour observations (nine pre-intervention, nine 3-months, and eight 9-months post-intervention) were conducted at three UW Health pharmacies.
Pharmacist Interviews
The purpose of the interviews was to understand how medication discontinuation orders are received and responded to by pharmacy staff, facilitators and barriers to discontinuing the orders in the pharmacy management software, and the impact of those orders on their workflow and workload. A total of 27 interviews with end-users were conducted (three interviews pre-intervention, three interviews 3-months, and three interviews 9-months post-intervention at each pharmacy).
Proactive Risk Assessment
A multi-step analysis process was used to conduct a proactive risk assessment that included: 1) generation of a process map iteratively refined through several full research team meetings, 2) identification of vulnerabilities and consequences associated with each step in the process map initially by the engineers, public health researcher, and pharmacists, and further refined by the physicians, 3) identification of actors (pharmacy staff, prescriber, clinic staff, patient, technology) involved with each vulnerability by the research team, 4) identification of vulnerability themes by the research team.
Principal Investigator
Co-Investigators and Collaborators
Research Staff
There was an immediate, significant, and sustained increase in the proportion of successful medication discontinuations after implementation. Introduction of CancelRx increased medication discontinuation from 34% to 93% post-implementation.
Clinic Type
Before implementation, primary care clinics had a significantly lower proportion of medications successfully discontinued in both the clinic and pharmacy as compared to specialty clinics (difference 17.7%, p < 0.001). CancelRx showed no differential effect between primary care and specialty clinics’ proportion of successful medication discontinuations (difference 1.6%, p = 0.219).
The final outcome of the study was to compare the average amount of time between discontinuation in the clinic system and pharmacy dispensing system pre- and post-CancelRx.
In the year prior to CancelRx implementation, the time required for a medication cancellation order to be discontinued in both the clinic EHR and pharmacy dispensing software varied—some prescriptions took several days while others were completed on the same day.
In comparison, after CancelRx implementation, medication discontinuations were all completed on the same day. This difference in pre- and post-CancelRx emphasizes that the instantaneous technology significantly reduced variation in the time to discontinuation.
Prior to CancelRx
When a patient is seen in an outpatient clinic, there are several opportunities for medications to be stopped or discontinued—medications that they should no longer be taking. A patient may indicate that they are “not taking” a medication on their own, a medication therapy may have ended on its own, like an antibiotic for a one-time illness, or a prescriber may stop the medication due to a clinical decision.
When a medication was discontinued, a task/message was generated, instructing the medical assistant (MA) or clinic staff to contact the patient’s pharmacy. This message was conveyed to the clinic staff through “Inbox” messages, specifically in the “Medication Discontinuation” folder. Prior to CancelRx, there was variability as to whether or not MAs knew that this folder (containing these messages) even existed. Some Mas appeared to be very knowledgeable about the process, while others were only alerted to it via the study. Similarly, there was variability in whether or not the MAs completed these tasks, and “followed through” with actually calling the pharmacy. Some MAs insisted that they contacted the pharmacy for every patient seen by their designated provider, and some MAs called on every patient regardless of the provider seen in the clinic. MAs often stated they contacted the pharmacy for some medications but not others, using clinical judgment to determine if a pharmacy needed to be contacted. Additionally, some MAs knew about the Inbox messages but said they did not have enough time or were not able to prioritize contacting the pharmacies regarding medication discontinuations.
Overall, there was a great deal of variability in the workflow/process surrounding medication discontinuation in the clinic prior to CancelRx and MAs stated that they received no formal training on the medication discontinuation process.
Post-CancelRx
CancelRx was implemented as part of a system-wide EHR update in October 2017. Overall, the workflow and systems surrounding the identification and discontinuation of medications did not change—providers (or MAs) were still able to discontinue medications and select a reason for discontinuation that indicated the pharmacy should be notified. The main difference, however; was that instead of creating a task for the MAs to contact the pharmacy through an Inbox message, SureScripts (a third-party health information network used to communicate between clinics and pharmacies), attempted to generate a CancelRx transaction that would communicate the information electronically. In order for CancelRx to be sent, the functionality must be “turned on” at both the clinic (sender) and pharmacy (receiver). For the purposes of this study, UW Health Pharmacies were able to receive CancelRx messages. If, however, the pharmacy functionality was not supported the CancelRx would “fail” and the system would create an inbox message task for the MAs to complete exactly the same as in the pre-period. If the CancelRx was sent to the pharmacy and successfully discontinued the medication, no further action was needed on behalf of the clinic staff/MA/provider. If, however; the pharmacy was unable to cancel the medication as detailed in the CancelRx message [described further below] a “failure” message was returned to the clinic via SureScripts and an Inbox message was created notifying the staff.
Prior to CancelRx
Pharmacists stated that they received cancellation messages infrequently, often approximating 3–5 each week. In theory, any pharmacy staff member (a technician, clerk, intern, or pharmacist) could receive these medication cancellation messages and discontinue them from the patient’s record. When a medication discontinuation message was received, the pharmacy staff member navigated to the patient’s medication profile, selected/highlighted the medication, and chose to discontinue/deactivate the item. This removed/canceled any future refills on the product. Additionally, a pop-up appeared, allowing the staff members to leave a comment or note as to why the medication was discontinued (i.e. replaced by new product, patient states not taking, allergic reaction, etc.).
In general, pharmacists stated they rarely communicated back to the clinic/provider indicating that the medication had been successfully discontinued (unless there was a question). Also, they stated that they may communicate this information to the patient if instructed to do so by the cancellation message, but many had assumed that the patient was aware of the changes and informed by the provider/clinic. When discussing the medication cancellation process with pharmacists, many interviewees stated they were unsure if technicians felt comfortable discontinuing a medication in the patient’s profile and may defer/communicate these messages to the pharmacist to utilize clinical judgment.
Post-CancelRx
After CancelRx implementation, the overall workflow for processing an electronic prescription did not change. There was, however; a change in the way the majority of medication discontinuation messages were communicated. Post-implementation of CancelRx, most medication cancellations messages were arriving at the pharmacy via CancelRx. Interviewees stated that they received cancellation messages much more frequently than prior to CancelRx, approximately 20–50 per week on average.
CancelRx messages were received at the pharmacy in the Inbound/Reception communications queue (the same location as new e-prescriptions). According to UW Health Pharmacy policy, these messages were only to be addressed and acknowledged by the pharmacist (not technicians or other pharmacy staff members). When a pharmacist clicked on a CancelRx message, a pop-up screen appeared. The CancelRx message contained information pertaining to the patient, the written and dispensed product, the prescriber, and whether or not the medication was currently being processed.
Many pharmacists commented on how they wished that the CancelRx message included the reason for discontinuation. After potentially investigating the message (e.g., going into the patient’s medication profile or electronic health record), the pharmacist would return to the CancelRx message and select “Remove from ICQ” [inbound communication queue]. Pharmacists said that it was unclear at first, but they learned through experience (and going to the patient profiles) that the CancelRx/SureScripts connection had already discontinued/deactivated the medication—there was no “undoing” the process. Their act of clicking the “Remove from ICQ” button was simply to attest that they had seen and acknowledged the medication was discontinued. This was also evident because after medication was cancelled via CancelRx it was locked and unable to sold or released to a patient.
If the CancelRx system was unable to automatically “match” the cancellation message with a prescription in the pharmacy system, the pharmacist could manually match the orders. Additionally, in the event the pharmacy was unable to match the prescription (perhaps in the instance of an old/outdated prescription more than several years old or if the prescription has been transferred out of the pharmacy), the pharmacist could indicate “No Match Found,” which removed the message from the inbound queue and sent a response to the originating clinic/doctor’s office.
At first, many pharmacists were frustrated by the sheer number of CancelRx messages they were receiving. They stated that most of the messages were meaningless in that they were for acute therapies (such as antibiotics) or for medications that had no refills (such as controlled substances).
Additionally, pharmacists/pharmacies also voiced frustration over the fact that once a CancelRx was received and a medication was cancelled using that method, there was no way to reverse the cancellation. This hard-stop safety functionality provided barriers when a pharmacy needed to re-bill for product after it was dispensed, or when the CancelRx was sent prematurely or unintentionally (often in the case of hospital discharges in which a patient was sent one prescription to the Outpatient pharmacy for immediate use and a second prescription to the patient’s usual community pharmacy for chronic use).
Overall, pharmacists recognized the value of this functionality in preventing discontinued medications from being released to patients. This highlights the need for well-designed technology that considers the end-user in design and implementation.
Front-line pharmacist and pharmacy leadership perceptions were compared using Epistemic Network Analysis (ENA). ENA is a quantitative ethnography technique to model the structure of connections within data. This technique provides insight into how individuals make sense of the world around them by describing the linkages found within discourse. ENA provides a systematic way to compare networks and understand how connections differ between people. First, codes were created to encompass the components of the SEIPS work system model: person, tasks, tools and technology, organization, and physical environment. Next, each sentence of the interview transcripts was coded using an automated coding software (ncodeR, 2018). We graphically modeled pharmacist and pharmacy administrators’ connections between cancellation messages (CancelRx) and work system components using ENA.
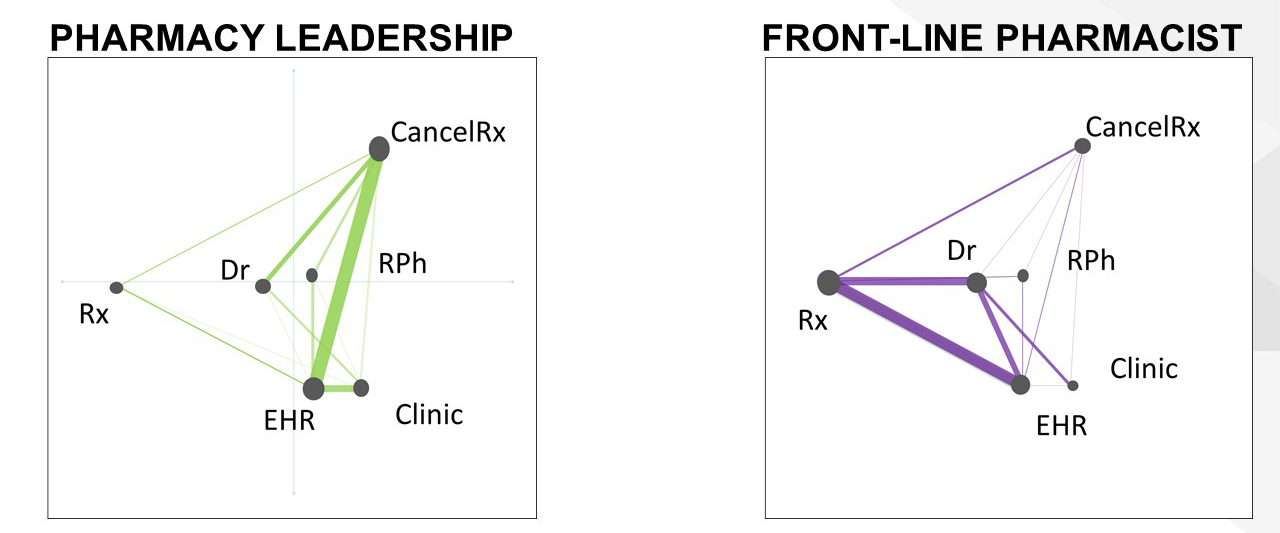
The qualitative data and ENA illustrated different connections amongst SEIPS components between pharmacists and pharmacy administrators. Dispensing pharmacists viewed CancelRx as just one communication tool in the scope of a larger medication discontinuation process. These participants perceived that the process of cancelling a medication required consolidating information from the providers, prescriptions, and the electronic health record. The pharmacist considers all of these components and attempts to make sure that they are all aligned.
Pharmacy administrators, removed from the day-to-day workflow of dispensing pharmacies, presented a rather narrow depiction of the medication discontinuation process and viewed CancelRx in an isolated way without recognizing interactions of CancelRx and work system components.
These results highlighted the importance of assessing implementation of new innovations in terms of an individual’s role within an organization. ENA allowed us to go beyond assessing just how pharmacists and pharmacy administrators view a novel Health IT innovation—but also how they viewed and framed the problem CancelRx was intended to solve. Ultimately, the findings emphasize end-user consideration when implementing a health IT functionality or any new innovation
A proactive risk assessment was also conducted in order to identify vulnerabilities and consequences associated with each step of the CancelRx process. Using the process map generated from the interviews and observations as a guide, 35 vulnerabilities that encompassed the clinic and pharmacy work systems were identified and organized into vulnerability themes.
Consequences for these vulnerabilities included clinic medication lists not being up to date, patient continuing to take a medication they should no longer be taking, inconsistent clinic work, medication discontinuation messages not communicated to pharmacy or unnecessarily communicated to pharmacy, important information not passed from the EHR system to pharmacy system, pharmacy medication list is not up to date, and increased workload for pharmacy.
Figure 7. Medication Discontinuation Process Map
View larger map image
The majority of themes involved multiple actors. For instance, an accurate clinic medication list was dependent upon the patient sharing information about which medications they were currently taking, clinic staff correctly documenting that information in the EHR, and proper interpretation of the medication list by the prescriber. Failure in any one of these steps could lead to the consequence of the medication list not being up to date or the patient continuing to take a medication that they should not be taking. Figure 7 above illustrates a revised process map that identifies where vulnerabilities may be located across the clinic, during handoff/communication, and in the pharmacy.
This study provides valuable insight into the impact of CancelRx on reducing medication list discrepancies between clinician EHR and pharmacy dispensing software. These findings illustrate the potential for health IT in mitigating risks for the dispensing of previously discontinued medications and decreasing the time in which these discontinuations are communicated. Additionally, the results demonstrated how CancelRx had varied impact based on the patient’s comorbidity status as well as the resources the originating clinic had access to (such as personnel). The study emphasized the importance of considering the environment in which new technological interventions are implemented—anticipating differences in resources and capabilities that impact implementation and adoption.
Although CancelRx has the potential to reduce medication discrepancies between clinics and pharmacies, it is clear that additional adjustments to both the IT functionality itself (e.g. closed-loop communication) as well as additional training and organizational policies for clinic and pharmacy staff that elucidates the roles of clinic staff, prescribers, and pharmacists in the medication discontinuation process will lead to improved medication safety outcomes for patients.
This study has several implications for practice: