13
March

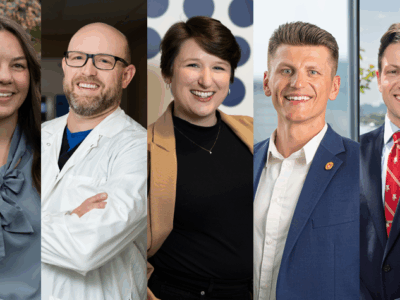
Alumni Brett Eberle, Nancy Gilbride, and Pat Cory weigh in on the news-making industry’s trends
By Katie Ginder-Vogel
Pharmacy benefit managers (PBMs) have been making headlines lately, with regulations to manage drug costs being discussed at state and federal levels.
PBMs, introduced in the late 1960s, are an intermediary between pharmaceutical companies, insurance companies, and pharmacies. They serve to negotiate drug pricing and distribution and manage formularies — lists of prescription drugs covered by an insurance plan — as well as establish an insurance company’s network of covered pharmacies.
If PBMs have been around for nearly 60 years, why are they in the news now? University of Wisconsin–Madison School of Pharmacy alumni in the industry — Brent Eberle (BS ’98), senior vice president and chief pharmacy officer at Navitus; Nancy Gilbride (BS ’90, MS ’93), principal and chief commercial officer at RxClarityGroup; Pat Cory (BS ’92, PharmD ’95), pharmacy benefits consultant, CoryPharm — visited the School of Pharmacy to share their insight on the evolution and future of PBMs.
Here are some of their discussion’s most salient points.
How have PBMs evolved?
In other countries, price controls at the federal level keep the costs of pharmaceuticals in check. The U.S., without those federal controls, instead gave rise to PBMs, which were developed to bring payers together to negotiate access to pharmaceuticals and pricing.
“What PBMs initially provided to the market, the functions that they served, addressed a significant cost savings opportunity for the payers of healthcare. These services were really valuable and really needed at the time. We went from the very manual process of paper claims filing with no discounts from the pharmacy and no ability to check for drug interactions or issues when medications were received across pharmacies,” says Gilbride.

When PBMs first entered the market, there was a great need and a clear value proposition. PBMs could provide claims processing, mail service, and a network of pharmacies, saving employers 15 to 20 percent.
“Now, benefit design and clinical programs have become incredibly complex, and several options are available for a plan sponsor, such as the application of maximum out-of-pocket payments, prior authorizations, and patient assistance programs, to name a few. There is an order of precedence to what rules are applied first when processing and pricing a claim,” Gilbride says. “The level of customization can be quite mind-boggling, certainly even more so as you move into the larger plan sponsors who cover Medicaid or Medicare populations.”
When PBMs started, one reason was to figure out how to process claims and move payments through the system more quickly. The industry created a trade organization that became The National Council for Prescription Drug Programs, through which pharmacies, payers, and the federal government agreed on standards that allow for that exchange of data.
“The pharmacy industry, including manufacturers, all agreed to these standards and still collaborate through the same process today,” says Eberle. “It helps transactions move along incredibly quickly.”
Each pharmacy transaction runs hundreds of calculations in less than a second.
“One of the things that surprised me when I got into the business is the degree of technology that’s involved,” says Eberle. “An individual pharmacy claim pulls in over 250 attributes. A lot of those are pricing attributes and plan design attributes that go back-and-forth in real time between pharmacies and PBMs.”
What are the greatest challenges and opportunities PBMs face today?
PBMs have increasingly been the focus of healthcare policy reform at both the state and national levels. Eberle says that pharmacy benefit reform is one of the few current issues with bipartisan support.
“There is broad agreement that something needs to be done,” says Eberle, who testified in front of the House of Representatives’ Subcommittee on Health on the issue in 2019. “The challenge today is that almost all of the players, with the exception of the patients and the payers in those boxes, benefit as drug prices increase, whether you’re a wholesaler, a pharmacy, or a traditional PBM.”

Those various supply chain entities benefit because their revenue generally comes from a percentage of drug sales. So as drug prices increase, their revenue increases, even if the percentage they receive decreases.
“There’s little incentive to actually manage costs and to bring lower-cost products to market,” Eberle added. “There’s several examples that we’ve seen where manufacturers have tried to bring a lower cost product to market but get pushed back all the way through the drug supply chain and ultimately aren’t successful.”
Since PBMs first entered the market, they have consolidated into a few large companies that manage the majority of health plans. But now, new types of PBMs, including virtual ones, appear to be returning to the original goal of PBMs, operating the way PBMs did when Eberle, Gilbride, Cory, and others began in the field. If these new organizations challenge traditional PBMs, that could lead to a more balanced market.
For example, Gilbride points to the effectiveness of PBMs focused on transparency, such as Navitus. Navitus pays pharmacies what it charges clients and gets paid through a disclosed administration fee back to the client, which separates the company’s compensation from drug pricing — Navitus doesn’t benefit as drug prices increase. She thinks that these newer PBM models are poised to grow.
“I’m doing work now with employers and brokers who want to move away from the Big 3 PBM companies that control 80 percent of the market, and am able to show them dramatic cost savings by moving to more transparent PBMs,” she says. “These new and existing players are gaining momentum in the market, so I think we are finally heading in a direction of better market balance.”

A common refrain of PBM reform includes the need for transparency.
“I think the challenge in trying to regulate transparency in drug pricing is that the industry has created multiple definitions,” says Eberle. “Will the regulation result in lower costs to patients and payers or is it simply adding costs by creating new administrative expense.”
The rising cost of healthcare — which increased about 5 percent per year between 2014 and 2020 — is often woven into conversations about PBM reform, even though they’re discrete issues.
“It’s squeezing different parts of the bubble,” says Eberle. “We’ve seen states come up with minimum pharmacy reimbursements, but then the pharmacy can’t agree to a discount agreement that’s less than that, so it will not necessarily lower the overall cost.”
How are pharmacists involved in the PBM and managed care industry?
Pharmacists, as medication and patient care experts, are key players in PBMs.
“There are endless possibilities in the managed care world and within pharmacy benefit management companies for trained pharmacists: medication dispensing and clinical operations, specialty pharmacy management, government affairs, contract compliance, marketing, sales and account management, prior authorization services, medication therapy management, and complex care management,” Gilbride says. “Another big area for pharmacists within PBMs or managed care is on the product development side, where the search for programs that drive to a lower net cost and/or better member care is prevalent.”
Eberle and Cory add that PBMs also offer jobs in mail pharmacy; pharmacy network contracting; pharmacy auditing; pharmacy affairs; formulary work; work with the analytics and underwriting teams; and fraud, waste, and abuse.
“Pharmacists in managed care organizations play a jack-of-all-trades role, working with various teams to interpret legislation, implement operations, and communicate with the C-suite.”
—Pat Cory
“Pharmacists in managed care organizations play a jack-of-all-trades role, working with various teams to interpret legislation, implement operations, and communicate with the C-suite,” says Cory.
Getting new generations of pharmacists involved in the space is how PBMs will continue their evolution to better serve patients.
“There is a need in our healthcare system for more people to understand the details of our existing drug distribution path,” he says. “The more we can educate on that and have a new generation of pharmacists who envision that supply chain in a new and different way, there’s opportunity.”