8
December

The University of Wisconsin–Madison School of Pharmacy’s Pharmacy Experts Webinar Series’ seventh installment focuses on population health and its principles, including and how they are applied within a rural health system, leveraging the expertise of pharmacists.
Watch and listen as School of Pharmacy alumni Christopher Barron (BS ’97), Tyler Prickette (PharmD ’17), and Tony Knutson (PharmD ’20) share how Fort HealthCare applies principles of population health, including its key initiatives, pharmacists’ roles, and best practices that promote population health initiatives.
Professor David Mott: Welcome to the seventh installment of our Pharmacy Experts webinar series. The title of our webinar tonight is Pharmacy’s Role in Population Health. I want to thank you for taking time this evening to join us for the webinar on this very interesting and important topic that will describe the ongoing popular population health program at Fort Healthcare in Fort Atkinson. It’s our UW School of Pharmacy alumni at Fort Healthcare who are at the cutting edge of population health programs in rural areas.
One of the main topics tonight will be how pharmacists in leadership positions and pharmacy departments in health systems can leverage their expertise to design, implement, and evaluate population health programs in rural communities.
My name is Dave Mott, and I’m the associate dean for advancement at the UW School of Pharmacy and I will moderate tonight’s webinar. This event is being sponsored by the UW School of Pharmacy advancement office. I want to acknowledge and thank Alissa Karnaky, our alumni relations and advancement coordinator; Anna Reinhart, our events coordinator; and Jasmine Loving, dean’s office assistant, for their work, marketing and producing this event.
Before we get started, I want to describe the process we will use for taking questions. First, the chat function is turned off for attendees. Second, due to the number of attendees, we will not be taking verbal questions. Instead, please use the Q&A feature on Zoom to type and submit your questions as you think of them. Since some of the questions may be the same across individuals, please feel free to click on the thumbs up icon to upvote the question. Then during the Q&A session, I will read the questions with the most upvotes for the panelists to answer. The webinar is being recorded and we will send you a link when the recording is available. We also will be sending you an evaluation of the webinar tonight. So let’s get started.
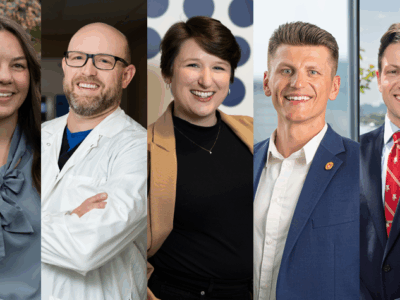
Our webinar panelists this evening are three incredible UW School of Pharmacy alumni, Chris Barron (BS ’97), Tyler Prickette (PharmD ’17), and Tony Knutson (PharmD ’20).
Chris Barron earned his BS degree in pharmacy from UW in 1997, and an MBA from Carroll University. Chris is the executive director of population health and clinical services at Fort Healthcare, an independent hospital and health system in rural South Central Wisconsin, and has been in this position since 2015. Chris leads Fort Healthcare’s internal and external population health and health equity strategies. Chris serves on the board of directors for the Wisconsin Collaborative for Health Care Quality, and as board representative to the collaborative’s health disparity initiatives.
Dr. Tyler Prickette earned his PharmD degree from UW Madison School of Pharmacy in 2017 and, earned his BPS certification in 2020. Tyler is the director of pharmacy for Fort Healthcare after joining Fort Healthcare in 2019. As a clinical pharmacist, and practicing in an ambulatory care world, Tyler’s role allows him to work throughout the health system to advance pharmacy practice in all avenues of health care for the benefit of the patient and the system. Tyler is involved in the community by being a co-chair of the Jefferson County Drug Free coalition and a member of the Jefferson chapter of the Knights of Columbus.
Dr. Tony Knutson earned his PharmD degree from the UW School of Pharmacy in 2020 and completed his PGY-1 residency at Fort Healthcare. He is a board-certified pharmacotherapy specialist as of July 2020. Tony currently is a clinical pharmacist at the McConnell Air Force Base in Wichita, Kansas. He recently made the move from Wisconsin, where he previously worked as a clinical pharmacist at Fort Healthcare. Tony has a strong passion for improving the transition of care across a patient’s health care experience and is continuing his relationship with FHC through contract employment to grow the primary care pharmacy service line by working directly with primary care physicians to improve guideline-directed medication access to patients in the community. Tony is an avid fitness enthusiast and continues to enjoy watching people reach their fitness goals through coaching Olympic lifting.
Thank you Chris, Tyler, and Tony for joining us this evening. So to get started Chris, what is population health and population health management and what does that look like at Fort Healthcare?
Chris Barron: Thanks for having us, Dave.
The widely accepted definition of population health comes from an article titled, “What is population health?” from doctors David Kindig and Greg Stoddart in a 2003 issue of the American Journal of Public Health. They describe it as a concept of health that, that is the health outcomes of a group of individuals, including the distribution of such outcomes within the group. These populations are often geographic and take health factors, determinants, and policies and programs take into account those things. So what we’re really talking about here are geographic denominators when we measure.
In our case, for the sake of measurement, we consider Jefferson County as our geographic denominator. We look at, what I’m showing here, again, is a graphic from the county health rankings, that shows what this model looks like in practice, health outcomes, how factors policies and programs is the way it is broken down there. We also consider this thing called population health management, which the American Hospital Association defines as the process of improving clinical health outcomes of a defined group of individuals through the through improved care coordination, patient engagement, supported by appropriate financial care models. So this, this is really a clinical denominator for Fort Healthcare patients or Fort Healthcare patients with diabetes for instances is the way we look at that.
So our, sorry, try this again, trying to advance the slide. Our mission, vision, and values at Fort Healthcare have been centered around population health and health equity since 2010. Really, and as you can see on our mission map here that depicts our well-defined population, our partners are depicted there. And the paragraph that I call out there really begins to recognize the impact of the various health factors on our community’s health. It’s a very community-focused message that extends beyond our walls, and really invites collaboration with our community.
Mott: How did you, as a pharmacist, come to lead population health at Fort Healthcare.
Barron: Coming up, I apologize, I’m stumbling a little bit. All right. Is my slide still up? So my role as executive director of population health at Fort Healthcare was established in 2015, and it encompasses population health, population health management, and health equity. I was asked to be the first that that time, I was the pharmacy director, and proven myself as an organizational level problem solver and had a track record of using analytics to drive improvement, had an aptitude for it, and had well-established relationships with medical staff. So we had their credibility and trust.
So although we had a very population health-focused mission and vision for about five years already, we had a new analytics platform that needed to be stood up. So that was my first task in this role, really. So I was I moved to administration at that time to an administration suite and reported to the CEO. I’m not a population health pharmacist, but a population health executive that happens to be a pharmacist if that makes sense. And actually stepped away from pharmacy for a few years. And it wasn’t until a few years ago that pharmacy and a few five other departments were brought back under me.
Mott: Speaking to our rural health students you have mentioned how, in many ways, population health is uniquely suited to rural health care. What do you mean by that?
Barron: Yeah, for sure. First of all, I grew up in a town about 10 miles from here called Milton, small town. I have roots in the rural communities we serve. And my perspective, rural really isn’t one of deficit but one of asset. We have a lot of assets in our rural communities, rural communities, the ones I know are proud and independent, we care for one another. Our mission map, again depicts many of those relationships. Our population is also of manageable size. It’s about 85,000 people in Jefferson County, so it’s not so massive we can’t really touch everyone through our health system, our health systems, the largest health system in the county and one of the largest employers. So we have a lot of touch points with our community. Even more so as we layer in our clinics and services, such as school nursing.
Mott: You mentioned programs as an essential component of population health. What are some recent or current programs or projects you’re working on? At a population health level?
Barron: Yeah, we’re just a little small-town hospital, but we tend to work some pretty big projects. I’ve co-authored and project directed a federal HRSA grant from the Health Resources and Services Administration under HHS, which is one of several grants we were working back in 2019. The grant I co-wrote and directed was a quality improvement grant called Improving Diabetes Care for Healthier Communities, focused on equitably improving diabetes care.
We also worked on a HRSA Network Development Grant that funded the consolidation of our charity Safety Net providers into a single more sustainable entity that’s on the path to become a federally qualified health center. We’ve partnered with researchers here at the School of Pharmacy. We’ve done projects with opioid prescribing with the School of Pharmacy and other partners. We’ve worked with the School of Nursing on biography initiatives. We’re working with UW Ophthalmology Researchers and the National Eye Institute to improve diabetic eye screening rates in rural populations. So those are a few of the projects that we worked on right now, or we’re building on our prior work with the Community Health Center to advance health equity by measuring and reducing health disparities between our populations.
Mott: The Improving Diabetes Care for Healthier Communities program had a pharmacy component. How did that come about? And how did that project go?
Barron: Yeah, having a background as a pharmacist, I know the value pharmacists can add when they’re at the table. So it’s so valuable to get us at the table for this discussion. So when I co-wrote that Improving Diabetes Care for Healthier Communities project, it broke into nine sub-projects. One of those is specifically about advancing primary care pharmacy services. I wanted to get that placeholder in there to ensure that was sort of a jumpstart for many of our services. And we’re building off the opioid focus we’re already embarked on with the UW School of Pharmacy. So we had, we had that model kind of in place. We had the next project kind of teed up, and we want to make sure we made pharmacy part of that. We had proven a pharmacist could add value, layered in the diabetes side is part of the approach to team-based care. And Tony can tell us a little bit more about that experience.
Tony Knutson: Yeah, thanks, Chris. So yeah, really, for me, coming in. And Tyler was in the position prior to me, so I kind of just took the work that Tyler was doing and also ran with it. But really, in terms of being part of the HRSA grant. Being able to collaborate and partner with our comprehensive care management team and diabetes education teams really gave us an opportunity to see the work that they were doing, and not duplicate any of the work that that was already being done. It also really increased our visibility as a healthcare partner to provider groups and the rest of Fort Healthcare. And it really kept us in the loop of what our organization goals were for this specific population. So it really gave us you know, a good idea of like where we needed to go with primary care services line.
Mott: The Rural Health track at the School of Pharmacy, you rotated at Fort Healthcare and ultimately completed a PGY-1 residency there I understand you had a residency project that was longitudinal and very population health focused. Can you tell us a little bit about that project?
Knutson: Yeah, absolutely. I’d say I mean, just because I’m partial, I’d say that my longitudinal project from my residency was the best project, obviously. But really, the aim of, of my project was to establish a pharmacy collaborative, which was aptly named the Pharmacy Collaborative of Jefferson County. And really, what we set out to do was create a collaboration between Fort Healthcare and our surrounding community pharmacies dispersed around Jefferson County. And the goal was really to open up lines of communication in hopes to gain insight into the needs of those community partners. We also wanted to establish ways we can help each other deliver more comprehensive care to our patients that we serve.
This work really continued after my residency, as I took over that primary care role, and played a part in being able to have those contacts and be able to communicate with those outpatient pharmacies about specific patients and making sure that your patients are adherence to their regimens, that sort of thing. And it actually has also impacted our inpatient side where we’ve been able to send discharge summaries to those pharmacies when medication changes are made, especially on med packaging and adherence packaging patients so that nothing is missed when they’re discharged back into the community.
Mott: Tyler, Chris has the C-suite, Tony has boots on the ground. Where’s your head at as director of pharmacy with Fort Healthcare population health initiatives?
Tyler Prickette: Absolutely. I think being a director of pharmacy really, really puts you in an advantage to understand both the administration’s perspective on what outcomes we’re looking to improve as an organization along with understanding the ins and outs of how pharmacy department should function, and how to best position some of your pharmacists to make impacts on those outcomes.
So like Tony said, I’ve been in the ambulatory pharmacist role, what we’re now calling primary care pharmacists, prior to him taking over that role, and it really gave me an advantage to understand what it takes to impact a population health management outcome. I was primarily focusing on pain management and had adapted along with our HRSA grant, to start working on improving diabetes management as well, really positioning Tony well to, like you said, hit the ground running and really make an impact on our patients that we’ll talk about later. And it just kind of couples from there. So we I get chances to build relationships with our C-suite leaders, other managers and look at organizational goals such as improving the blood pressure of our population, and trying to develop ways for us to take on these population health management outcomes and utilize our pharmacists team to the top of their license to improve the health and well-being of our community.
Mott: So evidence of improvement and other outcomes are important in population health management. Can you speak to any outcomes from pharmacy involvement with population health initiatives at Fort Healthcare?
Barron: Yeah, I can. And before I do that, I think I my slides can probably be seen now, right? Yes, we can see. So yeah, I apologize before I was partway there. And I didn’t click the second button. So before I do that, I’ll just show the graphic I had up before, which is that of the county health rankings, which speaks to health outcomes, health factors, and policies and programs, as well as our mission map here that speaks to our partnerships, our well-defined relationships with within the community or well-defined population, and then that population, focus population health focus mission, that begins to talk about those various determinants of health and how they impact the health of our population.
Now back to the data question. Yes, we do. We do collect a lot of data on various initiatives, and that becomes a key aspect of what we do at Fort Healthcare. I guess skip ahead here. So on the on the data side of what we do with improving diabetes care for healthier communities, we had a data scorecard we tracked on this. And we track performance over time on a variety of measures here.
In this view here, I blacked out some of the irrelevant ones to focus on two of them: an A1C less than 8 and A1C less than nine. And those are two areas we focused on as part of the team-based approach during the project. And as we can see, from grant year one to two to three, we saw some improvement. But more importantly, we really sustained improvement since that time and actually improved since then. Um, so that those are some of the data points we had at the big picture view of how pharmacy as part of a team could achieve some measurable outcomes. That, that we were tracking for sake of the grant, we track these for value-based purchasing at all, as well. So that’s become a real bright spot with our value-based metrics. Tony can add some case examples to this as well.
Knutson: Thanks again, Chris. I don’t know if you can switch to the next slide. Perfect. Excellent. Yes, we did want to share a little bit of clinic data that we gathered over the last year. So basically, all all the data that you’re seeing on the slide here is from January 1, 2023, through about September 2023. So our upper left chart shows the total number of visits that we did in that time, the blue pie piece is diabetes visits and follow ups. And then the red is all other patient visits. And you can see the diabetes patients certainly took up a big chunk of time and necessary, you know, visits and follow ups. The upper right chart shows some of our A1C data.
So we had 24 patients that were included in those 142 visits. And basically what you can see as an initial A1C, they were around 9.7. And we’ve got a nice trendline going down, which is what you want to see, especially when you’re following up so closely with these patients were first follow up, it was decreased in that second follow up, it was decreased even further. So looking fantastic there. And the lower left just to show that this is not just pharmacy work. This is a collaboration with many health partners, but specifically these 24 patients, we had a lot of collaboration with our CCM and diabetes education team. So you can see, you know, about half I was consulted alone, or pharmacy was consulted alone, most likely those were medication related things like med acquisition and things like that. But, you know, a lot of times we were collaborating with those CCM and diabetes education, and then the lower right, just wanted to show a breakdown of the distribution of insurance types. So we didn’t have any uninsured patients. But you can see the vast majority of our patients where they’re commercially insured, or Medicare. So and we’ll talk a little bit more about barriers to care a little bit later on here. So overall, really what I what what this shows is that in order to have a more significant impact on a disease state like diabetes, we really need a team approach with closer and more frequent follow ups with patients.
Mott: Data as is certainly impressive. So it sounds like the ability of pharmacists to engage in patient care activities in your clinics that move metrics that matter the most to administrators is a key component of the collaboration between administration and pharmacy. How are you making this sustainable for the system?
Knutson: That’s a really good question, Dave. And I think it comes down to the top right chart that Tony had showed and that’s getting the outcomes and primarily what we want to focus on it with having such a history of population health goals as a system. We’re really looking to try and make those impacts in the outcomes, and that comes back to value based reimbursement dollars for the system as well. So it’s really, really beneficial to have data and be able to show information like that top right corner because not only as we all know, pharmacists have struggled getting advantages billing, in clinic settings for a long time. I will say that we all know that’s also changing here soon with Wisconsin Medicaid, acknowledging pharmacists as providers here. So we’ll have more opportunities to make the sustainable in the future. But we’ve really focused and tried to accentuate those outcomes that we’re getting to justify having pharmacists in roles in the clinics. And again, it goes back to having that mission and vision focus of the organization where we can position our pharmacists to make an impact on our patients lives.
Mott: Barriers, so what have been some of the key barriers to your patients meeting their health care goals? And how have you as their pharmacist help them overcome those barriers?
Knutson: Yeah, I think one of the major barriers for us is, I’m the only pharmacist out there. And Tyler was the only pharmacist out there when he was out there. And we’ve got seven clinics that we cover, and I think about 14 providers. So having that as just one barrier. I mean, even if I go to one clinic, you know, a day per week, you’re still only in clinic every two to three weeks. So a lot of our you know, provider engagement can be impacted that way, but also being able to do in person patient visits. So a lot of our visits were via phone, which sometimes is more convenient for the patient. But it does take away a little bit of that body language feedback that you sometimes get from a patient. So you know that that was a little bit challenging.
For me, it was nice to be able to, you know, spend time on the phone with a patient, they can have their medications in front of them, and we can go through them one by one, which was great. And it allowed us to have quick conversations to do more frequent follow ups as well.
You know, the other thing for our patients is a lot of them are either underinsured or are lower income or fixed income. As you saw from the chart earlier, we had quite a few Medicare patients. And a lot of times these patients require a little bit more hands on with medication acquisition. So doing a lot of that for like medication manufacturer grants and manufacturer coupons just to get people on the right guideline directed therapies. And then we also dealt with a lot of health literacy challenges. So many of the patients that I was consulted on, didn’t fully understand their disease state or their medication. So providing that feedback and that education with those close follow ups really felt like it had a large impact for those patients.
Mott: Before about collaborations, what have been some of the key partnerships that you’ve developed within the organization that have helped with the success of the program?
Prickette: Yeah, I think first and foremost, the biggest relationship that’s helped us have such success is with our providers. Having the opportunity to get face to face with our outpatient providers, which especially as hospital pharmacists, primarily, we don’t typically get to do, being able to get ourselves on boots on the ground right in the clinics has been a big assistance to us being successful. Being able to be in their clinics and work directly with their patients, like usually right next to them, has really gained us a lot of favor with them and really show what pharmacists can do when put in those positions. So we’ve really made ourselves invaluable from that perspective.
The other partnerships we’ve made is with other department managers, whether these impact population health outcomes or not, we try and make ourselves the medication experts in every situation whether it has to do with the clinical side or medication acquisition or using our electronic health record efficiently. We try and build those partnerships by being looked upon colleague to to really make everybody’s lives easier, which ultimately improves patient outcomes. So.
And lastly, I think we, we really try and build partners with leadership, the more we interact not only as the department leader, but the more opportunities I give my pharmacists to interact with the leaders of our organization, the better they understand what our organizational leaders are trying to work toward. And we’re able to really meet the expectations of everyone.
Mott: Relationships, but we know that population health relies on building partnerships outside of the healthcare system. What are some of the partnerships that for health care has developed within the community? And how are they utilized to improve the population health goals of the organization?
Barron: Yeah, so I can, I can cover this one. And I’ll get to the slide in a moment here. But I spoke about our partnership with our Community Health Center Rock River Community Clinic, the network grant actually established a Rock River Health Care Network as part of that grant with eight community partners, which were one of those and that that work continues to this day. So working outside Fort Healthcare, we’re working at the community level with those partners to address needs in our community, many times for patients that aren’t seeing it for health care. So I’m a member of that Rock River Health Care Network steering team and we’re currently scoping out our next community project addressing other needs we’ve identified in our community health needs assessment.
But back to that, that Rock River Community Clinic work, my team has duplicated the measurement work we do here at Fort Healthcare. And we do that for Rock River community clinics. So I kind of failed mentioned as part of that project is condition of the network grant was to assure Rock River had an electronic health record as a condition of becoming a federally qualified health center. So we extended our electronic health record to the Community Health Center, as well as our analytics capabilities that me and my team provide. So we all the work we do here, we duplicate for them. So now we can measure how well Fort Healthcare population performs on a variety of health measures, and how well the Rock River Community Clinic population performs. And they’re very different population. They’re about an 80 percent Spanish speaking, Hispanic population. So now, we compare those two populations in our community and can actually identify and track health disparities, which is what you see here on the screen are our health disparity tracking. And we can work together now, to reduce those disparities over time, we actually sit on their their quality improvement team, we have a meeting tomorrow. And we use this data that to drive improvement on the community level, and actually really to to start a lot of great conversations in our community about what health disparities look like in our community, and really starts to rally support around reducing those.
So the work we do here, we didn’t just make this up, I’d love to say we did. But this is modeled after work being done by the Wisconsin Collaborative for Healthcare Quality and their partners, and we’re a member of that we work closely with them. As we mentioned in the intro, I’m on their board of directors and work on their health disparity strategy there. But they’ve Wisconsin’s done a lot of great work in this in the space on health disparities. So there’s a lot of great models out there. If you look at WCHQ.org health disparity, you can see how the things are tracked at the state level. We essentially brought that locally and did that and started tracking these things locally with our other health partners. Our work in the future is to do this internally as well.
So on the topic of health disparities, the thing I’d like to cover I know it’s Dave’s favorite graphic here, talking about health disparities, and health equity. One way we talk about this, when we talk about with our teams and with others, it’s always easy to pick the low hanging fruit when we’re looking at care gaps and approaching efforts to improve health. When we do that, what we tend to do is reinforce or exacerbate health inequities in our community. So we use this to kind of explain that to people that we need to think creatively how we reach further up those trees as we as we layer in additional supports for those populations that might need those additional supports so everyone in our community can achieve their best health outcomes.
Prickette: I think I’ll add just a little bit to this is that, you know, other partnerships that we’ve built. In my bio, I mentioned that I’m a part of the Jefferson County Drug Free Coalition. And we’ve had, I think the partnerships that we built internally allow us to the opportunity to also get involved in the community and things like that. So initially, when we started our ambulatory care program, it was very pain management focused and that drug free coalition is something that has meant a lot to our community and is working again, on prevention and meeting the mission vision of Fort Healthcare, but done from a very pop public health and population health standpoint. So to be able to be a voice for health for healthcare, and an organization like that directly in the community is also really awesome opportunity.
Knutson: Yeah, just as a another quick aside, you know, the collaborative that I that we developed during my residency, has paid dividends and made connections. So one of our community pharmacies was starting to develop a wellness program. And we have a community health and wellness program at Fort Healthcare. So being able to connect those two, so they could work together is a huge benefit to the community as well. So that, again, they’re not duplicating work, and they can probably have a bigger impact together than just by themselves.
Mott: Awesome. Chris, you have the slide about the data up there. I mean, I would think that having you know, the data that you guys are able to collect showing these comparative outcomes and trends over time that has to be incredibly impactful to others in the community to facilitate those partnerships with Fort Healthcare.
Barron: Oh, yeah, definitely. This data has, it’s facilitated so many conversations in our community about what this looks like many times. When we talk very abstractly about health disparities or social determinants of health, it’s, it’s hard to put that into context. And when you show it with data, it adds that level of context that we can show that the outcomes for our patients are different than the outcomes or other patients are the measures that lead to outcomes for other patients are very different. And then using that becomes very powerful to improve things. So not only working at, say, the community clinic level, helping them reach their patients, but collectively working on efforts to say, “Wow do we support mammography vouchers in our community to reach all these populations?” So we have a voucher program that provides vouchers for women that need mammography services across anyone in Jefferson County. We just did a large campaign for Breast Cancer Awareness Month and are evaluating that data now to see how that’s impacted or closed some of the disparities we see. So yeah, very, very impactful.
Mott: Some of these metrics are going to require some best practices in pharmacy. So Tony, what are some of the pharmacy best practices that you’ve utilized within the practice?
Knutson: Yeah, I think, really, you know, in the beginning part of the program, it was really letting providers know that I was in clinic with them, like being present. Actually doing some prospective patient reviews on patients that they were going to see that day with possible medication optimizations and consultations just to kind of get the ball rolling a little bit, maybe garner some of their support and confidence in the program. Because I think that’s really the biggest thing is making sure that the providers know what you can offer. So that’s those the big thing.
One thing that I do have to say is if you’re trying to bill for your services, you can’t double book a visit with provider and you the same day and bill for both; you’ll end up you know, making the providers kind of mad about that stealing their billing opportunity. So, just as an aside. I’m, we were lucky enough, we don’t bill for our services. So I could see a patient same day. But I felt like if I didn’t say that might come up later on.
So you know, the other thing is, you know, going above and beyond for providers and just trying to take work off of their plate, right? You know, that is one way to garner their support and really make your program take off is adding that value to them. And then, of course, the collaborative practice agreement question is naturally going to come up. And certainly, you want to use CPAs, to expand your practice, the way that we formulated our workflow early on, didn’t really require that because we kind of circumvented that by proposing orders to providers, and we had pretty good relationships with the providers to start to be able to do that but still something we’re continuing to work on and develop as we’re building this program to make it more sustainable for the future.
The other thing that I really, you know, feel pretty strongly about is having a good understanding of insurance, and manufacturer grants and, and programs to help patients afford their medications. I think that, you know, of those visits that we had and the consults that we had from riders, a lot of them just don’t know how to get a medication covered. And if you can take that off of their plate, in the beginning parts, that’s going to really make you stand out. And that’s that, that got a lot of attention from our providers, when we’re able to get medications through when nobody else could. So having that resource catalog of those is, is really big.
And then of course, Chris would be really disappointed if I didn’t mention this: collect data, whatever you do, just collect something, even if it’s not right, and you need to change course, at some point, collect something so that you can understand the impact that you’re having.
Barron: Data only gets better when you start using it. Start somewhere.
Mott: Chris, you you have this expertise in population health, and you’ve been at this for a while. So what do you believe is the most significant factor or factors that’s led to the success of Fort Healthcare’s population health initiatives?
Barron: I gotta say pharmacists, though, but we’ve proven our value here, beyond just what you might traditionally consider pharmacy and my role in the C suite, and Tyler’s role in pharmacy leadership, and Tony’s boots on the ground. We, we it’s beyond, you know, providing services. It’s building programs, it’s tying these things together with the community. It’s using our skills in many different ways to solve organizational and community level challenges, and really getting in tune with what those things are. So getting aligned with where the heads in the C suite are, getting aligned with what the challenges in the community are, with the community health needs assessment, which were a big part of that.
But the skills we have as pharmacists don’t always need to be limited to medications, I mean, that just the problem-solving skills of having good rapport with providers and data and it and things like that, you can apply them in different ways.
Mott: So what can other pharmacists — we have pharmacists here attending tonight — so what can other pharmacists do to take on population health, or population health management projects, with their facilities that they’re working at or within their communities?
Barron: I can start off and Tony and Tyler pick up on that as well. But kind of back to what I just said, we’re where we started, a lot of it was really building our brand, building our credibility here at the organization. And that was about really becoming aligned with organization-level initiatives and priorities. And the more you’re aligned with that, the better position you’re in to be able to raise your hand and say, hey, I can help with that.
Becoming best friends with the quality department, too, early on. When I was a pharmacy director, that’s one of the first places I spent a lot of time is with our quality manager at the time. And we did a lot of great projects together that started out to be very pharmacy focused projects, medication safety, but we built our brand and our credibility from that and it extended and other bigger projects down the road. And then lastly, a hit back on Tony and data and my thirst for data, but really assessing how we measure success. And instead of measuring success by hey, we provide a service or we provide access to something or we get an outcome. And really starting to align with moving measures and trying things if the things we’re doing aren’t producing the outcome we want to do, how do we change the things we do? I don’t know if Tyler or Tony have anything to add to that.
Prickette: Yeah, and I, the biggest thing I want to emphasize is that when we started our ambulatory care program to get pharmacists more out, outside of the walls of the hospital, none of our pharmacists had any particular training in ambulatory care. I think when we talk a lot about it, we talk about residency programs and getting more experienced through that. Tony’s been the first residency trained pharmacist that we’ve had out in the clinic. Prior to me, it was another pharmacist that’s been on our team for 10 years. We just had that drive to want to work with patients and I had the relationship with the providers. So it a lot of the skills that we have inherently as pharmacists that we’ve learned in school, all put us in a really good position to impact patient lives and have active listening conversations with our patients to understand what’s impacting them, and then have the knowledge base or the understanding of our resources to figure out how to help them. So we don’t need necessarily any particular training to start making an impact, it’s, again, building those relationships with providers, and having that drive to want to make an impact on patient lives.
Knutson: Yeah, and I can just round us out as the boots on the ground guy. And just say that, you know, sometimes when we’re developing these programs, we get caught up in formulating the perfect plan to execute and get the work done. And sometimes you just have to start somewhere. And I feel like that’s kind of what we did with this program is, you know, we just started, we started doing the work and opened it up to the providers, and it really caught fire and, you know, gained a lot of a lot of favor with the providers because of the services that we were, we were offering.
And it does require you like Chris said, to stay flexible, if things aren’t working, or if you’re not getting the outcomes that you’re looking for, you might have to change directions. But you know, always been open to feedback, and especially from, you know, the C suite folks, and, you know, presenting your data, and, you know, hoping that the data that you’re collecting is offering good outcomes. So, but really, it’s about getting started. Just start.
Mott: Let’s take a look at some of the questions that have been submitted by some of our attendees. If you have questions, please submit them into the Q&A function on Zoom. So we’re talking about, you know, developing programs, implementing them and using pharmacists skills in different ways. There’s a couple of questions that relate to exploring ways to incorporate pharmacy technicians into Fort Healthcare’s population health programs. So could you just talk a little bit about how you’re utilizing technicians to help facilitate the implementation of some of the programs?
Barron: Yeah, we would love to. Do you have any? That’s the challenge right now, is it? Honestly if if we had technicians to spare, I think we would love to do something with that right now. That’s, that’s the challenge. And one of the challenges in rural health care delivery is we work with the team we have and the team we have right now is more pharmacists than technicians, but we would love to have technicians and expand those roles.
Prickette: We’ve got a great strategy in pharmacy to build a really strong technician tree, not just a technician career ladder, hopefully allowing them to not only grow in their roles to beyond the standard pharmacy technician duties, but getting them involved in patient care from medication histories to medication access programs, like Jenny had said in the Q&A. Love to have that help because as much as pharmacists have a wealth of knowledge on the medication access programs, they’re not always the ones that need to be doing that. And I think it’s a perfect spot to utilize pharmacy technicians, with the caveat being if you can find the technicians that are interested in it.
I also think data analysis is a really, really cool opportunity that technicians could have to get involved in, doesn’t necessarily take a whole lot of background, it just takes a thirst for learning more and learning something new. A lot of the data work that we get involved in, we didn’t have a huge background in before we started playing around with the numbers. So it’s something that we can easily teach to a pharmacy technician and have them involved from an analytics perspective as well.
Mott: Question, interesting question. How do you reach out to bilingual patients or non-English speaking patients? I know you mentioned the clinic, Chris, just kind of curious challenges and how you overcome those challenges?
Barron: Yeah, it’s challenging. And we continue to look at ways we can get better at that right now. We we utilize a translation service right now. And that’s available across our organization. For translation, we’d love to hire more bilingual staff, as we see opportunities to do that. Our Community Health Clinic, of course, they have many more bilingual staff than we have, so they’re able to reach many of those patients, when we do events that we know are going to, to be focused on those populations. We have translators present as well, our latest mammography, that we had translators. But that is on our radar, we do want to make sure we’re providing equitable access to all populations in our area. That includes when we do things electronically. We’ve recently did a refresh on our on our internet page, and we’re building more and more bilingual aspects into that as well. So it is on our radar. And we’re everyday trying to get better with that.
Prickette: This isn’t a paid advertisement for the School. But I think that, you know, the School of Pharmacy does a really good job of training the next generation of pharmacists to interact through translators. We have a student with us recently that went through that and was able to do a medication history using our translation services. And she actually utilized a lot of the skills that she had in the communications class to, you know, make direct eye contact with the patient and just use the iPad service to talk with the patient. And then the provider came in and was able to pass right off to the provider to have the same, have their conversation too. So we do utilize those services really well. But I think, you know, even as a student, it can sometimes be a little bit more nervous to get involved at the bedside, especially when it comes to you know, patients that are non-English speaking primarily. But the school sets, pharmacists have well to communicate efficiently and with a human aspect in those situations where we might have a lot of communication barriers.
Knutson: And in our primary care, pharmacy services, we don’t shy away from consults for non-English speaking patients, we actually tried to encourage our providers to send those patients to us only had a handful of of those consults, but utilizing the translation service via phone, we were able to, you know, communicate with those patients and, you know, whether or not it had a huge impact on their health outcomes. You know, we still were able to communicate and, you know, get medication access in some of those cases.
Mott: There’s another question I think, is really interesting. So when we think about rural health, rural, rural counties, rural communities, you know, access to providers and stuff. So what, what do you guys see as the role of telehealth or video conferencing for patient visits to promote access when patients are in maybe more remote areas?
Knutson: To be honest, I think that video calls would be probably one of the best things for a program like we have one because then you can see what the patient’s home situation is. They can, you can see them pull out their medications, you can see how they maneuver around their home. So So you can, you can kind of get a little bit more insight into how they are at home versus them coming into a clinic and seeing you in person. So I do think that there’s a lot of value added there. For those visits for sure,
Prickette: We ended up Oh, go ahead, Chris.
Barron: I was going to say that to support that, it is recognized that many rural areas have poor access to broadband. And that’s something being worked on actually at the community level right now, that’s come out of our community health needs assessment. So there is work being done at the county level on improving broadband access, and we’re able to influence some of that work.
Prickette: Yeah, I think the only thing I was going to add was, you know, video visits are great, but we have a lot of patients that want to either come into the clinic and see us face to face, we’re a lot of the contact that they want to have with healthcare providers. They don’t necessarily always want to drive to Madison, or Milwaukee or Janesville, even just because of, you know, the traffic increases significantly from their perspective. So they like coming to our clinic, because it gives them social interaction from, you know, their communities of 1,000 folks where they see the same couple of people all the time. So we like to have that connection with them. But we really try and offer all those opportunities wherever the patients at whether it’s phone, video or face to face. So a lot. And that’s where I think rural health has the opportunity to really flex and meet the patients where they’re at, because we get that direct feedback from from patients. They want a video visit, they’ll tell us and we’re able to make that happen.
Mott: Like this always comes down to a lot of questions about funding. And you know, Tony, you mentioned a little bit about billing for visits and things so that the question from an attendee is how, how is your population health program funded?
Barron: Yeah, so so right now much of our funding is, much of our perspective is through achieving mission and vision related goals. We get some value-based reimbursement from many of these items. Diabetes care is one of those that’s on our value contracts we look at, and outcomes there. And by being able to achieve some of those outcomes with pharmacists, that frees up provider time to provide other care. So that’s right now, the way we’re looking at it, definitely we want to go down that road of getting paid for many of these services. But again, we wanted to start somewhere. And that’s kind of where we are right now.
Mott: Right, last question, we have, I think, is a great question just about the overall approach here. So the question is, how does sport healthcare work on advancing population health among the residents of Jefferson County, who don’t have any connection with your health system? You know, Chris, you you have that map that you showed in the second slide of the community all working together. Can you talk a little bit about kind of what you’re doing for patients who aren’t part of the health system?
Barron: Yeah, so and I was alluding to that a little earlier, but our work with what we call the director of our health care network, and there’s eight partners, they’re going to look over at my poster here and I can read them off there. So we have Fort Healthcare. We have the greater Watertown Community Health Foundation, Jefferson County Health and Human Services. We’re gonna have Madison Area Technical College, Rainbow Hospitals, Rock River, Community Clinic, Watertown Department of Public Health, and Watertown Regional Medical Center. So we work with all those entities on trying to solve broad population level challenges.
And many of that those things start with their community health needs assessment that we do in partnership with those same entities. So we we have a pretty unique approach to the Community Health Needs Assessment in that respect. And then we work together on on the challenges within that actually just stalking to a data analysts from the foundation yesterday from the Watertown Foundation, about trying to aggregate our data a little better and go beyond what we’re doing and, and so we’re in those discussions. Again, we started somewhere we have what we have between us and Rock River. We have a lot of other bits and pieces of it and piece by piece. I think we’re going to find ways to sew that together.
Mott: We are at time. So that is our webinar for this evening. And again, thank you, Chris. Thank you, Tyler. Thank you, Tony, what a great discussion about population health management.
Also, I want to thank our attendees for attending the webinar. And please look for an email with a link to an evaluation survey so we can obtain your feedback about tonight’s webinar. Also, please check out the School of Pharmacy’s YouTube channel to watch the previous six pharmacy experts webinars.
Also, if you have an idea for a future pharmacy experts webinar, please feel free to send that to me or Alissa Karnaky at the School of Pharmacy and we can begin to pursue perhaps producing that topic in a future webinar and other alumni engagement activities.
Please check out the latest edition of DiscoveRx, the School of Pharmacy’s digital publication.
Also please look for information to participate in the next installment of virtual trivia night to raise funds for Pharmacy Alumni Association scholarships on February 6. So everyone please stay safe and healthy and have a nice evening and on Wisconsin. Good night, everyone.