This is an accordion element with a series of buttons that open and close related content panels.
Why is it important for a health system to consider what the surrounding communities are doing related to opioid stewardship?
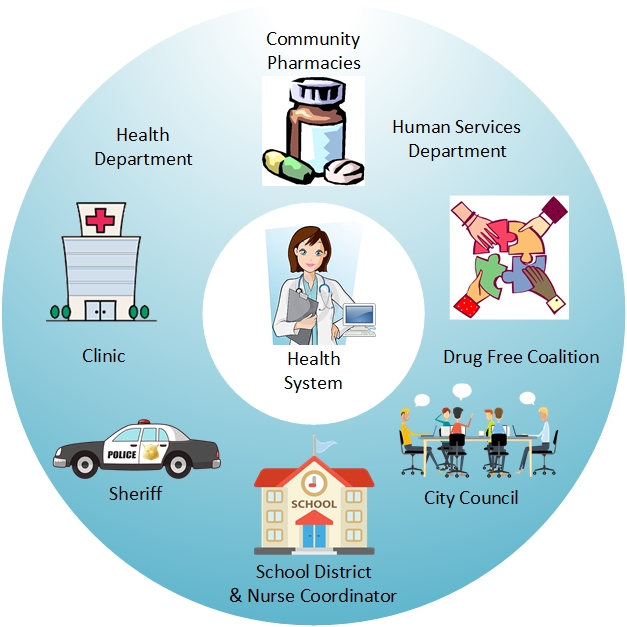 The opioid crisis is too big for health systems alone to address comprehensively. The opioid crisis is multifaceted and affects many aspects of communities including: emergency departments, operating rooms, neonatal intensive care units, police, fire, EMT, family practice, behavioral health, dental, pharmacies, and schools. Many health systems are making progress implementing opioid stewardship to improve the safety of opioid prescribing and expand opioid use disorder treatment, but these efforts alone cannot address all aspects of the opioid crisis across the community. Therefore, health systems need to collaborate with community partners with shared goals and complementary expertise or treatment capacity to have a larger impact in their communities.
The opioid crisis is too big for health systems alone to address comprehensively. The opioid crisis is multifaceted and affects many aspects of communities including: emergency departments, operating rooms, neonatal intensive care units, police, fire, EMT, family practice, behavioral health, dental, pharmacies, and schools. Many health systems are making progress implementing opioid stewardship to improve the safety of opioid prescribing and expand opioid use disorder treatment, but these efforts alone cannot address all aspects of the opioid crisis across the community. Therefore, health systems need to collaborate with community partners with shared goals and complementary expertise or treatment capacity to have a larger impact in their communities.
Gaps in available opioid-related treatment options or services can be filled through partnerships with the community. In some instances, opioid-related resources or programs don’t exist within a health system. To fill the gap, the health systems may need to look outside the box and join forces with community organizations to offer patients these resources. Module 3 discussed how health systems should conduct an opioid stewardship needs assessment to identify the gaps. In addition to considering how opioid stewardship is being addressed within the health system, it’s important to conduct an environmental scan of the surrounding communities served by the health system.
An American Hospital Association 2020 publication focused on opioid stewardship measurement offers the following approach related to conducting an environmental scan to identify existing resources within the health system, as well as in the surrounding community or county, related to opioid stewardship.
- What services exist internally?
- What is the capacity to offer new services or improve/expand/enhance existing services?
- What services/initiatives exist within the community?
duration:
00:03:31
Listen to Audio Clip
How an opioid stewardship team at a rural Wisconsin health system involved the community when conducting an opioid stewardship needs assessment
Clip from Podcast with Sarah Pagenkopf, Director of Pharmacy Services, Fort Health Care
00:44:37
Listen to Podcast
Full Interview with Sarah Pagenkopf, Director of Pharmacy Services, and Tyler Prickette, Clinical Pharmacist at Fort HealthCare, including:
- getting buy-in from leadership to initiate opioid stewardship
- conducting a gap analysis
- identifying a champion leader
- setting goals and
- offering lessons learned and advice for pharmacist colleagues in rural areas settings
duration:
00:02:32
Listen to Audio Clip
The importance of considering what is happening in the surrounding community when defining the opioid stewardship needs
Clip from Podcast with Nicole Green, Director-Ambulatory Pharmacy Services, ThedaCare
Listen to Podcast
Full Interview with Nicole Green, Director-Ambulatory Pharmacy Services, and Dan Cunningham, an Ambulatory Care Clinical Pharmacist at ThedaCare
- Highlights the role of a pharmacist in opioid stewardship efforts, including:
- Provider education through a CME presentation and academic detailing initiative focusing on 8 clinics in rural areas
- Identifying opioid-related risks to inform opioid stewardship
- How they have been able to support the pharmacist’s time spent on opioid stewardship
- Reflections on lessons learned and advice for pharmacist colleagues in rural areas, such as how this role is not specific to ambulatory pharmacists, but rather, can be done by any pharmacist
What community partnerships are important for a health system to develop related to opioid stewardship?
While every community is different, some common important partnerships that health systems should consider developing related to opioid stewardship are with:
- behavioral health treatment services,
- community retail pharmacies,
- law enforcement,
- county or municipal public health/ human service departments, and
- community coalitions to prevent and address substance use disorders
Behavioral health treatment services
Health systems in rural areas often do not have behavioral health staff and, therefore, forming partnerships with behavioral health treatment services and professionals in surrounding communities can facilitate opportunities for health system providers to refer patients for care.
The Wisconsin Department of Health Services supervises Wisconsin’s public substance use services system. All 72 counties are responsible for delivering services and providing for the well-being, treatment, and care of individuals living with substance use concerns. Services are often delivered in partnership with community-based agencies and organizations. Health systems should explore opportunities to collaborate with county-provided behavioral health substance use treatment.
Community Retail Pharmacies
 These pharmacies are freestanding pharmacies that are not affiliated with your health system (i.e., Walgreens, Hometown, CVS). Strengthening the link between health system pharmacists, prescribers and community pharmacists is critical for optimizing opioid stewardship across the community.
These pharmacies are freestanding pharmacies that are not affiliated with your health system (i.e., Walgreens, Hometown, CVS). Strengthening the link between health system pharmacists, prescribers and community pharmacists is critical for optimizing opioid stewardship across the community.
Community pharmacists have important roles in addressing the opioid crisis.
Examples include:
- Helping to prevent diversion of opioids by recognizing signs of opioid misuse by patients (e.g., multiple prescriptions from different physicians)
- Supporting the safe use of opioids by identifying inappropriate prescribing or hazardous drug combinations that physicians may not be aware of (e.g., opioid analgesics combined with benzodiazepines)
- Checking the WI prescription drug monitoring program (or PDMP) before dispensing an opioid prescription, and if the pharmacist has questions about whether to dispense the opioid medication, community pharmacists will contact the prescriber
- Provide patients with information on risks associated with opioid medications, proper storage and disposal of medications, and the harms (and illegality) of sharing medications with other people
- Dispensing the opioid antagonist naloxone, which has been shown to save lives when made available to opioid users and their families or other potential bystanders to an overdose; provide guidance about its use and even legal protections for bystanders to an overdose that customers may not be aware of
- Providing naltrexone injections or dispensing buprenorphine as a treatment for opioid use disorder
- Future potential roles for community pharmacists include dispensing methadone to patients in partnership with an opioid treatment program and implementing an opioid call-back program, in which pharmacists call patients 2-3 days after an opioid prescription is dispensed to ask about pain management, opioid storage, and disposal of unused opioids
However, community pharmacists often face multiple barriers which make it challenging for them to optimize their contributions to opioid stewardship. For example, community pharmacists often report a lack of clinical connection to other healthcare professionals. Many do not have access to medical records, which leads to a lack of information and hinders their ability to view patients comprehensively. Additionally, these pharmacists are often constrained by time. Due to the busy nature of community pharmacies, they may find it difficult to closely examine prescription opioid use or address concerns with individual patients or prescribers.
Some suggested ways that health system pharmacists can work with community pharmacists to overcome the opioid-related barriers they face include:
- promoting open communication between prescribing provides and community pharmacists
- extend health system training on opioid stewardship topics, such as naloxone, to community pharmacists and technicians
- invite community pharmacist to join opioid stewardship committee
- explore opportunities for the health system to sharing opioid-related information as part of the e-prescription – for example, whether the patient has an opioid agreement on file
Related to coordinating opioid use disorder treatment among health system providers, there are emerging practices that involve retail pharmacies providing opioid use disorder treatments on-site in the pharmacy. Recent pilot research is exploring pharmacies as a site for methadone dispensing.
Law Enforcement
 Law enforcement agencies, including county sheriff’s departments and local police departments, are important partners for pharmacy and opioid stewardship teams within health systems to connect with because opioid medications are controlled substances, and their prescription, dispensing, storage, possession, use and abuse are all subject to federal and state laws. Additionally, patients presenting to the health system with opioid-related health concerns are often also involved with law enforcement. In some cases, law enforcement and health systems have conflicting priorities related to individuals with substance use disorder treatment needs and there are often limitations on being able to share crucial information due to patient confidentiality or legal considerations.
Law enforcement agencies, including county sheriff’s departments and local police departments, are important partners for pharmacy and opioid stewardship teams within health systems to connect with because opioid medications are controlled substances, and their prescription, dispensing, storage, possession, use and abuse are all subject to federal and state laws. Additionally, patients presenting to the health system with opioid-related health concerns are often also involved with law enforcement. In some cases, law enforcement and health systems have conflicting priorities related to individuals with substance use disorder treatment needs and there are often limitations on being able to share crucial information due to patient confidentiality or legal considerations.
The Minnesota Hospital Association offers a Health Care and Law Enforcement Collaboration Road Map, which is a broad framework of how to care for patients involved with law enforcement. The framework has a goal of enhancing communication and collaboration between health care and law enforcement. The road map includes best practices and compiled resources that provide leadership and direct care staff with tools to build relationships and improve collaboration between health care and law enforcement. Suggested best practice examples include:
- scheduling routine operational meetings between law enforcement and health care teams,
- prior notification from law enforcement and communication to hospitals of the results of public safety assessments,
- health care organization has a process in place to provide information sharing with law enforcement, which complies with HIPAA and State Health Records laws.
It is important to coordinate with law enforcement related to diversion programs, strategies for medication disposal, such as drop boxes in police stations, and naloxone programs, such as equipping law enforcement agencies with naloxone for direct administration by officers and first responders, when warranted.
County or municipal public health or human service departments
These departments are responsible for promoting the health of county or municipal residents, and many have opioid-focused initiatives to prevent opioid harms. In some instances, these departments provide substance use disorder treatment services, such as medications for opioid use disorder. The Wisconsin Department of Health Services provides links and resources to local county and tribal public health departments and agencies across the state.
Community coalitions to prevent and address substance use disorders
In addition to county or municipal public health services or resources, community coalitions to prevent and address substance use disorders exist in many communities across Wisconsin and work towards prevention and treatment of opioid harms. These coalitions are often organized by a county public health agency or a local non-profit organization.
 There are many resources at the national, state and local levels available to support such coalitions. For example, in 2017, the state of Wisconsin received a 2-year grant from the federal Substance Abuse and Mental Health Services Administration (SAMHSA) titled State Targeted Response to the Opioid Crisis (STR) to provide local opioid-related coalitions with resources to implement specific strategies aimed at reducing the availability of and access to opioids for nonmedical purposes and to prevent the consequences of opioid abuse. Funds were intended to enhance local coalition-led efforts related to preventing opioid abuse, rather than supplanting current or ongoing prevention efforts.
There are many resources at the national, state and local levels available to support such coalitions. For example, in 2017, the state of Wisconsin received a 2-year grant from the federal Substance Abuse and Mental Health Services Administration (SAMHSA) titled State Targeted Response to the Opioid Crisis (STR) to provide local opioid-related coalitions with resources to implement specific strategies aimed at reducing the availability of and access to opioids for nonmedical purposes and to prevent the consequences of opioid abuse. Funds were intended to enhance local coalition-led efforts related to preventing opioid abuse, rather than supplanting current or ongoing prevention efforts.
70 substance abuse-related coalitions located in 43 counties, including 10 tribal coalitions, received the funding.
Coalitions used the funds to support numerous prevention strategies, such as Drop Boxes, Take-Back Events, and Naloxone training.
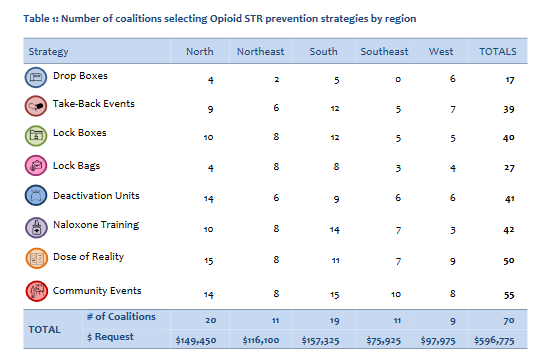 This report can be a resource for pharmacists and colleagues in health systems who are exploring whether such a coalition exists in the communities that they serve. It also provides examples of work that coalitions have done in partnership with health systems.
This report can be a resource for pharmacists and colleagues in health systems who are exploring whether such a coalition exists in the communities that they serve. It also provides examples of work that coalitions have done in partnership with health systems.
Two examples of opioid-related coalitions in rural Wisconsin counties are:
![]() The Jefferson County Drug Free Coalition is a community organization that works to prevent and reduce alcohol and drug misuse among youth and the greater community through county wide collaboration. Pharmacy team members from Fort HealthCare have been involved with the Jefferson County Drug Free Coalition for a few years and are actively involved in a working group focused on addressing issues with the opioid crisis.
The Jefferson County Drug Free Coalition is a community organization that works to prevent and reduce alcohol and drug misuse among youth and the greater community through county wide collaboration. Pharmacy team members from Fort HealthCare have been involved with the Jefferson County Drug Free Coalition for a few years and are actively involved in a working group focused on addressing issues with the opioid crisis.  For more details about this partnership, listen to the podcast for this module. One example of the work that the coalition has done in partnership with Fort HealthCare and others, is the publication of an Opiate & Drug Awareness Toolkit – a Resource for Prevention, Treatment and Recovery. This comprehensive booklet provides valuable information (e.g., local stories local resources for treatment options) to better educate the community about the ongoing opioid epidemic and other drug use.
For more details about this partnership, listen to the podcast for this module. One example of the work that the coalition has done in partnership with Fort HealthCare and others, is the publication of an Opiate & Drug Awareness Toolkit – a Resource for Prevention, Treatment and Recovery. This comprehensive booklet provides valuable information (e.g., local stories local resources for treatment options) to better educate the community about the ongoing opioid epidemic and other drug use.
duration:
00:02:00
Listen to Audio Clip
Description of the Jefferson County community coalition addressing substance use disorder
Clip from Podcast with Emi Reiner, Public Health Nurse, Jefferson County Health Department & Project Coordinator for the Jefferson County Drug Free Coalition & Tyler Prickette, Clinical Pharmacist, Fort Health Care
Listen to Podcast
Full Interview with Emi Reiner, Public Health Nurse, Jefferson County Health Department & Project Coordinator for the Jefferson County Drug Free Coalition & Tyler Prickette, Clinical Pharmacist, Fort Health Care
- How Fort HealthCare became involved with the County Drug Free Coalition
- Examples of activities that Fort HealthCare has done with the coalition
- Advice for making similar connections between health systems and communities in rural areas
The Sauk County Partnership for Prevention is an alliance of community members and local organizations that are dedicated to preventing youth vaping, youth alcohol use, and prescription drug misuse for residents of all ages. The Partnership is working on a variety of initiatives to help all of our community members reach their full potential, such as Safe Storage and Disposal of Prescription Drugs
What are strategies for health systems to develop relationships with organizations in the community?
There are many approaches that pharmacists and opioid stewardship teams at health systems can take to identify opportunities to develop relationships with organizations in the communities they serve.
Community organizations are often eager to engage with pharmacists and health systems, as they value their expertise and unique perspective.
- Explore online whether there is an opioid-related community coalition in the county(ies) served by your health system.
- If an opioid-related community coalition already exists, engage with the group and participate regularly in meetings to share and learn what the health system and community are doing in this area.
- Identify and connect with community-based organizations who seek to reduce the risk the opioid epidemic poses to the communities served by the health system.
- Often organizations hold regular meetings that are open to anyone to attend.
- Invite community partners to become part of health system committees, including opioid stewardship committees.
- Organize an informal meet-and-greet event and invite organizations to attend. This would be an opportunity for the health system to share with the community the efforts they are making related to opioid stewardship and explore partnering with organizations.
- Seek out and participate in community-based opportunities related to opioid stewardship in the communities served by the health system.
- Examples include a county-organized drug take-back event or a naloxone training for patients and families at a local community center.
00:01:23
Listen to Audio Clip
How a health system first became involved with a community coalition addressing substance use disorder in the county they serve
Clip from Podcast with Emi Reiner, Public Health Nurse, Jefferson County Health Department & Project Coordinator for the Jefferson County Drug Free Coalition & Tyler Prickette, Clinical Pharmacist, Fort Health Care
Listen to Podcast
Full Interview with Emi Reiner, Public Health Nurse, Jefferson County Health Department & Project Coordinator for the Jefferson County Drug Free Coalition & Tyler Prickette, Clinical Pharmacist, Fort Health Care
- How Fort HealthCare became involved with the County Drug Free Coalition
- Examples of activities that Fort HealthCare has done with the coalition
- Advice for making similar connections between health systems and communities in rural areas
What is an example of a health system that has connected with and collaborated with partners in their county around opioid stewardship?
Listen to a podcast episode detailing an example of how a rural Wisconsin health system engaged with a county coalition regarding opioid stewardship.
Fort HealthCare’s engagement with the Jefferson County Drug Free Coalition


00:15:38
Description:
- Interview with Tyler Prickette, Clinical Pharmacist at Fort HealthCare, and Emi Reiner, Public Health Nurse and Project Coordinator for the Jefferson County Drug Free Coalition discussing:
- how Fort Health Care became involved with the Jefferson County Drug Free Coalition
- examples of activities that Fort HealthCare has done with the coalition, and
- advice for making similar connections between health systems and communities in rural areas
Where can I find additional guidance about connecting with community organizations?
A resource that provides detailed guidance on health system engaging with community partners related in opioid stewardship is:
- The College of HealthCare Information Management Executives (CHIME) put together an Opioid Playbook which has a chapter on Community Outreach and Collaboration.
This chapter looks at different types of collaborations among different organizations and entities and provides real world examples of such partnerships.
There are several resources targeted to rural communities and addressing the opioid crisis. These may offer guidance for health system and community partnerships:
- Rural Community Toolbox
In May 2018, the Office of National Drug Control Policy (ONDCP) stood up the Rural Opioid Federal Interagency Working Group (IWG) to help address the opioid crisis by improving coordination of and reducing potential overlap among the federal responses in the nation’s rural communities. The Federal Rural Resource Guide to Help Communities Address Substance Use Disorder and Opioid Misuse was released in 2018. The most recent Federal Rural Resource Guide was released in February 2021. This website takes the Guide from PDF to an interactive online tool. It is operated under a contract with the University of North Dakota Center for Rural Health. It serves as a guide to the resources that can help make a difference in rural communities. It offers tools to empower rural community leaders to assess the causes and impact of substance use disorder and find federal programs to help them build strong healthy drug-free rural communities. - Centers for Disease Control and Prevention Rural Health Policy Brief – Preventing opioid overdoses in rural America – suggestions for addressing opioid crisis in rural areas. In addition, the following resources can assist providers and communities in efforts to reduce misuse and overdose: CDC’s rural health website and the Guideline for Prescribing Opioids for Chronic Pain resource page
- The Rural Health Information Hub’s Prevention & Treatment of Substance Use Disorders in Rural Communities Toolkit provides evidence-based examples, promising models, program best practices, and resources that can be used to implement substance abuse prevention and treatment programs.