This is an accordion element with a series of buttons that open and close related content panels.
How have national leaders described the importance of pharmacists in opioid stewardship?
The Centers for Disease Control and Prevention (CDC) and the American Pharmacists Association (APhA) promote the unique ways in which pharmacists can contribute to addressing the opioid crisis.
In conjunction with the publication of the 2016 CDC Guideline for Prescribing Opioids for Chronic Pain, a brochure was issued focusing on the role of pharmacists in opioid stewardship:
 “Pharmacists and prescribers share a common goal of ensuring safe and effective treatment for patients. The CDC Guideline for Prescribing Opioids for Chronic Pain emphasizes patient safety and encourages prescribers and pharmacists to collaborate in integrated pain management and team-based practice models. Pharmacists and prescribers should apply the guideline and work collaboratively to optimize pain management while preventing opioid use disorder and overdose. Establishing and maintaining collaborative working relationships improves patient outcomes.” (CDC, 2016)
“Pharmacists and prescribers share a common goal of ensuring safe and effective treatment for patients. The CDC Guideline for Prescribing Opioids for Chronic Pain emphasizes patient safety and encourages prescribers and pharmacists to collaborate in integrated pain management and team-based practice models. Pharmacists and prescribers should apply the guideline and work collaboratively to optimize pain management while preventing opioid use disorder and overdose. Establishing and maintaining collaborative working relationships improves patient outcomes.” (CDC, 2016)The American Pharmacists Association (APhA) issued an advocacy statement on Prescription drug misuse and abuse highlighting the pharmacist’s unique position to address this crisis:
In 2017, the Deputy Director of the National Institute on Drug Abuse (NIDA) of the National Institutes of Health addressed pharmacists about their roles in curbing the opioid crisis at the American Association of Colleges of Pharmacy (AACP) annual meeting.
“For pharmacists, being on the “frontlines of coprescribing” positions them to be readily involved in the care of pain patients. Dr. Compton highlighted novel practice strategies specific to pharmacist and pharmacy involvement:
- Expanded roles of pharmacists in protecting the community from diversion
- Integration with Prescription Drug Monitoring Program (PDMP) data systems
- Balancing the needs of pain patients while minimizing opioid overexposure
- The use of partial Rx fills as a potential prevention method
- “Current pilot research on pharmacies as a site for methadone dispensing”(https://www.pharmacytimes.com/view/the-opioid-crisis-what-can-pharmacists-do)
The NIDA Deputy Director expanded on the role of pharmacists in addressing the opioid crisis, highlighting the significant potential of pharmacists to make a positive difference, Promising Roles for Pharmacists in Addressing the US Opioid Crisis.
What roles can health system pharmacists play in opioid stewardship?
Pharmacists working in health systems have unique expertise, training and skills set to contribute to addressing the opioid crisis in numerous ways. National professional pharmacy organizations as well as pharmacy researchers have identified the multiple ways in which pharmacists have been involved in opioid stewardship efforts within their health systems and also advocate for an expansion of these roles.
In 2020, Mobilizing pharmacists to address the opioid crisis: A joint opinion of the ambulatory care and adult medicine practice and research networks of the American College of Clinical Pharmacy (AACP),was published.
The joint opinion states that pharmacists play an integral role on opioid stewardship teams. The authors suggests that pharmacists can:
- Develop and implement evidence-based opioid treatment plans
- Develop opioid order sets, prescribing protocols and guidelines
- Initiate and modify non-pharmacologic and non-opioid therapies
- Conduct prospective and retrospective case reviews
- Develop and implement opioid taper plans
- Evaluate high-risk drug/disease combinations
- Develop and implement controlled substance agreements
- Interpret qualitative and quantitative toxicology results, and
- Monitor for opioid misuse by patients and healthcare providers
(https://accpjournals.onlinelibrary.wiley.com/doi/10.1002/jac5.1331)
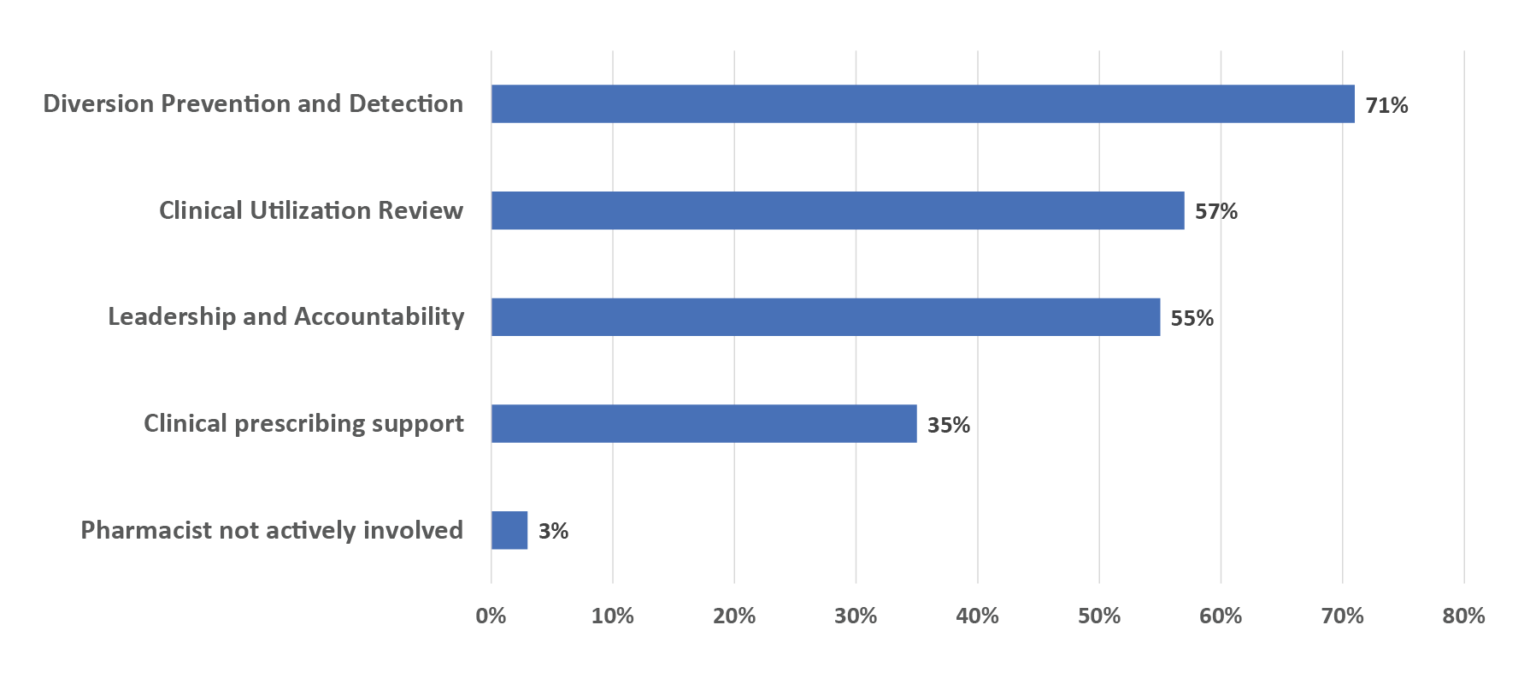
A 2018 American Society of Health-System Pharmacists national survey of pharmacy practice in hospital settings identified pharmacist activities and involvement in opioid stewardship programs (% = frequency of reported activity):
Additionally, specific opioid stewardship roles have been suggested for pharmacists practicing in hospitals or health system settings. A 2014 study highlighted the role they can play in identifying opioid toxicity, supporting appropriate opioid prescribing and preventing diversion of opioids.
A 2019 article, “The opioid crisis: Origins, trends, policies, and the role of pharmacists,” emphasizes pharmacists’ specialized training and unique qualifications to lead or participate in opioid stewardship initiatives.
Additional examples of strategies pharmacists may use to address opioid crisis:
Role and strategies focused on patients
- Collaboration with healthcare team on opioid exit plans and discharge planning
- Management of pain clinics in primary care settings under collaborative practice agreements
- Participation in provision of medication-assisted treatment
- Provision of medication reviews and/or medication therapy management
- Provision of counseling and education on appropriate pain management
Interventions with Other Healthcare Professionals
- Education of prescribers and other health professionals concerning appropriate pain and opioid management
- Provision of academic detailing
- Recommendations to prescribers prior to issuing prescriptions (or prior to dispensing) (Chisolm-Burns et al., 2019)
Module 7 expands on the pharmacist role in educating other health professionals, patients and the community about appropriate pain management and opioid management.
00:02:20
Listen to Audio Clip
Example of pharmacists’ role in implementing a clinical decision support tool related to opioid stewardship
Clip from Podcast with Tyler Prickette, Clinical Pharmacist, Fort Health Care
Listen to Podcast
Full Interview with Sarah Pagenkopf, Director of Pharmacy Services and Tyler Prickette, Clinical Pharmacist, at Fort Health Care
- Highlights 3 opioid stewardship initiatives that the Clinical Pharmacist has taken the lead on implementing:
- Opioid tapering service in family practice clinics
- Training providers and frontline staff on newly implemented EMR-based opioid clinical decision support too
- Expanding Medication Assisted Treatment
- Reflections on lessons learned and advice for pharmacist colleagues in rural areas
Pharmacists as leaders of opioid stewardship efforts in health systems
Pharmacists in health systems are often well-positioned to lead opioid stewardship initiatives. Pharmacists can initiate opioid stewardship activities and take on the role of championing the work within the health system and getting buy-in from leadership. Alternatively, pharmacists can lead by kick-starting the initiative and forming a team of colleagues, including providers and others who have influence with the health system leadership and become the face of the leadership.
Encouraging expansion of pharmacist role in opioid stewardship
There are numerous examples of pharmacists who have been contributing to and leading opioid stewardship in health systems for many years. A 2019 article reviewing pharmacists’ practice roles related to the opioid crisis found that pharmacists are taking active roles in opioid stewardship programs and initiatives. However, some experts are encouraging continued expansion of the pharmacist role in innovative opioid stewardship efforts by capitalizing on their existing skill sets and knowledge.
(00:02:12)
Listen to Audio Clip
Description of how pharmacists can contribute to opioid stewardship
Clip from Podcast with Nicole Green, Director-Ambulatory Pharmacy Services, ThedaCare
Listen to Podcast
Full Interview with with Nicole Green, Director of Ambulatory Pharmacy and Dan Cunningham, ThedaCare
- Highlights the role of a pharmacist in opioid stewardship efforts, including:
- Provider education through CME presentation and academic detailing initiative focusing on 8 clinics in rural areas
- Identifying opioid-related risks to inform opioid stewardship
- How they have been able to support the pharmacist’s time spent on opioid stewardship
- Reflections on lessons learned and advice for pharmacist colleagues in rural areas, such as how this role is not specific to ambulatory pharmacists, but rather, can be done by any pharmacist
What are examples of pharmacists implementing opioid stewardship in health systems serving rural areas?
Examples of pharmacists’ contributions to opioids stewardship are provided from three different Wisconsin health systems that serve rural communities:
- The Veterans Affairs Medical Center in Tomah, Wisconsin
- Fort HealthCare, based in Fort Atkinson Wisconsin serving Jefferson County, and
- ThedaCare, based in Appleton, Wisconsin and serving both urban and rural areas spanning 17 counties including the Fox Cities area (Appleton, Neenah), Berlin, New London, Shawano, Waupaca, and Wild Rose.
Each of these health systems has a unique set of resources and capacity to implement opioid stewardship.
1. Veterans Affairs Medical Center in Tomah Wisconsin
This case example is from a highly-resourced health system that has prioritized optimal pain management and opioid stewardship over the last several years. For health systems with fewer resources or those who are in the earlier stages of developing opioid stewardship, this case example offers a vision and roadmap for a potential role for pharmacists in opioid stewardship. Consider how a similar pharmacist role could be developed in your setting with the resources available.
Examples from the field: VA Medical Center in rural Wisconsin
This VA facility has a full-time clinical pharmacist who focuses on pain management. One facet of this position is to participate in this VA facility’s Opioid Safety Initiative Committee (OSI), which is a 7-member interdisciplinary committee including the clinical pharmacist, a physical therapist, a performance improvement nurse, a pain provider, a primary care provider, mental health representative, and a suicide prevention representative. The OSI Committee was developed in VA facilities nationally in 2013 to reduce the over-reliance on opioid analgesics for pain management and promote the safe and effective use of opioid therapy when clinically indicated. The OSI Committee at each facility looks different; some are run by pharmacists and others by medical providers or mental health professionals, but all are encouraged to be interdisciplinary.
The committee meets weekly as a group for an hour and a half and does in-depth patient chart reviews and makes recommendations to providers in the chart under an opioid risk review note. Prior to meeting, each committee member reviews the charts and then comes together as a group to discuss their recommendations from each of their areas of expertise, such as medication or pain. The pain pharmacist is the co-chair of this committee along with the primary care provider and is responsible for writing the chart review notes completed, leading the meeting, and coordinating any follow-up with providers that is identified from the reviews.
The list of patients that are reviewed by the committee is generated in a number of ways. Most come from a dashboard accessed by members of the committee (mainly the pain pharmacist or informatics nurse) and others are from data information pulls by the facility’s informatics pharmacist.
1. All veterans who are on an opioid and a benzodiazepine medication, as well as all of the patients who are on greater than 90 or previously 100 MEDDS are reviewed on an annual basis.
2. A performance improvement nurse, who is on our committee, monitors the annual drug screens that are done in our facility and reviews them to make sure are they appropriate, and if they aren’t, she looks to see if the provider followed up on them. The committee is a net that catches some of those patients who fell through the cracks on appropriate follow-up and intervention after a drug screen without substances prescribed or with non-prescribed substances present.
3. There is a consult feature in our EHR that providers can use to ask the committee to review a particular patient if they have a concern for a veteran because of an aberrant urine drug screen, or if they have questions about a particular patient scenario.
4. Patients are also identified by their risk through either the Risk Index for Overdose or Serious Opioid-Induced Respiratory Depression (RIOSORD) score or other VA created risk dashboards. Those that are identified as high risk also have reviews completed regarding safety and risk mitigation considerations.
Having an interdisciplinary committee has helped to create a shared responsibility for the recommendations offered and encourage and support providers in their prescribing and treatment. Additionally, it has been helpful for providers to get buy-in from patients when they share with patients that an interdisciplinary committee of met and discussed their case and made recommendations.
2. Fort HealthCare
Listen to a podcast episode about the role that a clinical pharmacist played in implementing opioid stewardship in a rural Wisconsin health system.
Discussing a clinical pharmacist’s role in implementing opioid stewardship in a rural Wisconsin health system

00:22:42
Description:
- Interview with Sarah Pagenkopf, Director of Pharmacy Services, and Tyler Prickette, Clinical Pharmacist, at Fort HealthCare.
- Highlighting 3 opioid stewardship initiatives that the Clinical Pharmacist has taken the lead on implementing:
- opioid tapering service in family practice clinics
- training providers and frontline staff on newly implemented EMR-based opioid clinical decision support tool
- expanding Medication Assisted Treatment
- Reflecting on lessons learned and advice for pharmacist colleagues in rural areas
3. ThedaCare
Listen to a podcast episode about the role a pharmacist played in implementing opioid stewardship in a health system serving rural Wisconsin communities.
Discussing a pharmacist’s role in implementing opioid stewardship in a health system serving rural Wisconsin communities

00:24:56
Description:
- Interview with Nicole Green, Director of Ambulatory Pharmacy Services, and Dan Cunningham, Ambulatory Care Clinical Pharmacist, at ThedaCare:
- Highlighting the role of a pharmacist in opioid stewardship efforts, including:
- provider education through CME presentation and academic detailing initiative focusing on 8 clinics in rural areas
- identifying opioid-related risks to inform opioid stewardship
- Discussing how they have been able to support the pharmacist’s time spent on opioid stewardship
- Reflecting on lessons learned and advice for pharmacist colleagues in rural areas, such as how this role is not specific to ambulatory pharmacists, but rather, can be done by any pharmacist
How can you justify the time a pharmacist spends on additional pharmacy services related to opioid stewardship?
Establishing a new pharmacist position to focus on opioid stewardship or adding new opioid stewardship responsibilities or clinical services to an existing pharmacist’s role will require getting buy-in from health system leadership. This can be particularly challenging for health systems serving rural communities who often have fewer resources and smaller pharmacy teams.
Modules 2 and 3 provide guidance and resources for obtaining support from health system leadership for initiating stewardship activities in general. Seeking approval for a pharmacist to spend (a portion of) their time on opioid stewardship may be a component of that larger effort to seek buy-in.
Strategies might include:
- Emphasize how the pharmacist-led opioid stewardship work contributes to population health by addressing the opioid crisis in the community. Describe how the opioid stewardship work is in alignment with the health system’s mission and goals to create a healthy community. Module 8 goes into greater detail about establishing partnerships with the communities served by the health system.
- You do not necessarily need to characterize the opioid stewardship initiatives as revenue-based proposals, but rather as something that is needed to address a national public health crisis that is impacting all communities.
- Ask for permission to conduct a short term (e.g., 6-month) opioid stewardship pilot project that an existing pharmacist or pharmacy resident who has a knowledge of medication safety or pharmacy and therapeutics could work on.
- Track project successes (e.g., reduced number of patients on high MMED prescriptions) to demonstrate to the leadership the value of the pharmacist’s contribution. Module 5 provides guidance on using EHR data to measure opioid stewardship outcomes
- Document feedback from providers to demonstrate their perspective on the added value of the pharmacist’s work.
- Highlight other benefits, such as contributing to the community-wide efforts to prevent opioid harms and save lives.
- Present to leadership the benefits of a pharmacist supporting providers in enhancing their opioid prescribing practices, such as through a pharmacist-led opioid tapering project. Show how pharmacists can offer the added benefits of sharing responsibilities with physicians and offloading part of the care burden, freeing up physicians to treat more patients. If possible, highlight the potential cost-savings of pharmacist time vs. physician time.
- Another strategy for obtaining support from leadership is to identify external funding opportunities to support program development and the role a pharmacist or a pilot project on opioid stewardship activities. This type of funding can support getting an opioid stewardship project off the ground and establish its presence. Oftentimes, once the value of a program is recognized by leadership, there is motivation to expand that program. Potential funding mechanisms to explore include:
- Federal grant opportunities (i.e., Health Services Research Administration, SAMSHA)
- Professional Pharmacy organization grant opportunities for innovative pharmacy practices (i.e., AACP innovative technology)
- Pharmacy resident project funding opportunities
- Community coalitions with funds to support opioid stewardship work
00:02:30
Listen to Audio Clip
How to get buy-in from leadership to support pharmacists’ time dedicated to opioid stewardship
Clip from Podcast with Nicole Green, Director Ambulatory Pharmacy Services, ThedaCare
00:24:56
Listen to Podcast
Full Interview with with Nicole Green, Director Ambulatory Pharmacy Services, and Dan Cunningham, Ambulatory Care Clinical Pharmacist, ThedaCare
- Highlights the role of a pharmacist in opioid stewardship efforts, including:
- Provider education through CME presentation and academic detailing initiative focusing on 8 clinics in rural areas
- Identifying opioid-related risks to inform opioid stewardship
- How they have been able to support the pharmacist’s time spent on opioid stewardship
- Reflections on lessons learned and advice for pharmacist colleagues in rural areas, such as how this role is not specific to ambulatory pharmacists, but rather, can be done by any pharmacist
00:05:56
Listen to Audio Clip
How to get buy-in from leadership to support pharmacists time dedicated to opioid stewardship
Clip from Podcast with Sarah Pagenkopf, Director of Pharmacy Services, Fort Health Care
00:22:42
Listen to Podcast
Full Interview with Sarah Pagenkopf, Director of Pharmacy Services, and Tyler Prickette, Clinical Pharmacist, at Fort Health Care
- Highlights 3 opioid stewardship initiatives that the Clinical Pharmacist has taken the lead on implementing
- Opioid tapering service in family practice clinics
- Training providers and frontline staff on newly implemented EMR-based opioid clinical decision support tool
- Expanding Medication Assisted Treatment
- Reflections on lessons learned and advice for pharmacist colleagues in rural areas