This is an accordion element with a series of buttons that open and close related content panels.
How can I make the case that opioid stewardship is important?
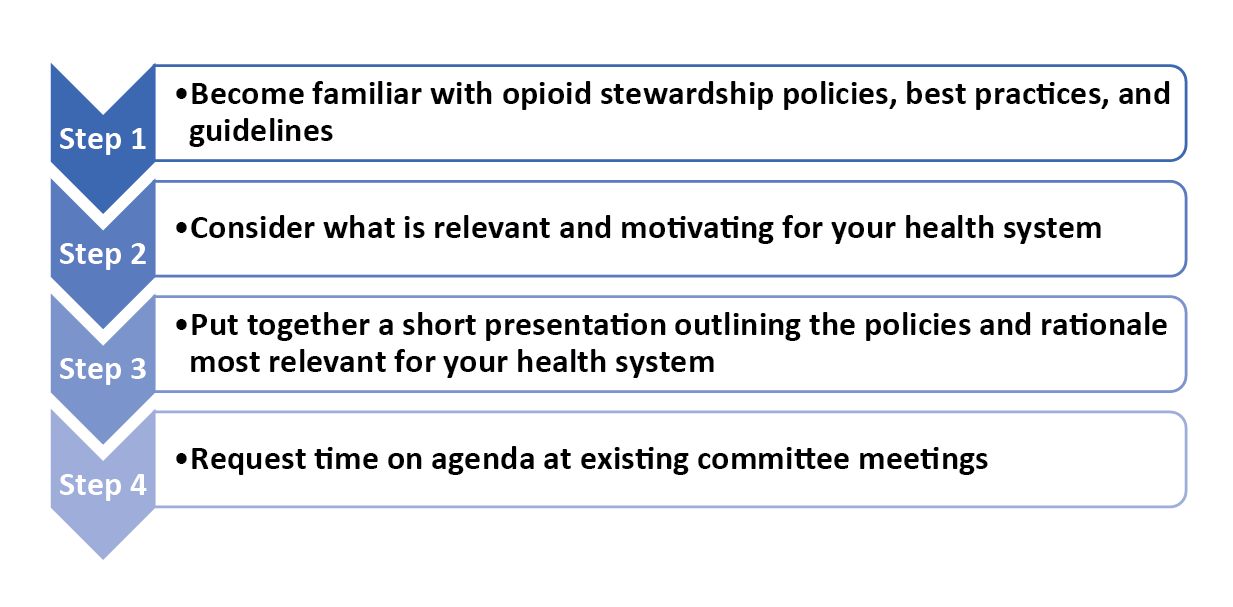 An important first step in making the case to health system leadership or colleagues that opioid stewardship is important, is to become familiar with the opioid stewardship policies, best practices, and guidelines.
An important first step in making the case to health system leadership or colleagues that opioid stewardship is important, is to become familiar with the opioid stewardship policies, best practices, and guidelines.
Module 2 provides a rationale for why health systems should prioritize opioid stewardship and highlights the opioid stewardship policies, guidelines and best practices.
Consider which particular rationale(s) for prioritizing opioid stewardship would be most relevant and influential for your health system. Think about what is important to the health system leadership in other practice areas. For example, you may consider the following:
- Is your health system focused on maintaining accreditation with the Joint Commission or other bodies?
- Does your health system prioritize quality improvement?
- Is opioid stewardship consistent with your health system’s mission?
Once you have identified the rationale that will resonate with leadership, develop a short presentation which outlines the opioid stewardship policies that are relevant for your health system and links them with the rationale for opioid stewardship. If possible, share some preliminary data on opioid prescribing to illustrate the need to address opioid stewardship. Module 5 provides further guidance on exploring data within the Electronic Medical Record.
Consider existing committees within your health system that would likely have an interest in, or be impacted by, opioid stewardship (e.g., Medication Safety, Pharmacy & Therapeutics, Medical Staff Lead Committees, or even Quality Based/Patient Safety Committees.) Once you have identified potential committees to approach, request to have 5-10 minutes on the agenda of an already-scheduled committee meeting to present about the importance of opioid stewardship and organizational data on opioid stewardship metrics at your health system.
This approach has several advantages in rural health systems, where providers and frontline staff often have multiple commitments to existing committees related to other issues: (1) it does not require an extra time-commitment, as they had already planned to attend the meeting, and (2) pharmacy presence at these meetings will help to secure provider buy-in, which in rural health systems is often key for obtaining buy-in from the administration and leadership.
A potential opportunity to raise awareness about the need for opioid stewardship is in response to an opioid-related crisis or event related to quality of care, regulatory compliance or an unexpected adverse event. By encouraging the organization to reflect on this situation and consider it on a deeper level, the pharmacy team and colleagues can foster a climate for change. For example:
When making the case about the value of opioid stewardship to your health system, it is important to think outside of the box about the benefits of opioid stewardship. There are many potential non-monetary benefits to implementing opioid stewardship, such as improvements in safety, efficiency, reducing readmissions, return to office or emergency room visits. Module 4 has additional guidance about how to get buy-in from leadership to form an opioid stewardship leadership team.
00:04:01
Listen to Audio Clip
An example of an opioid-related concern that motivated a rural Wisconsin health system to initiate opioid stewardship
Clip from Podcast with Sarah Pagenkopf, Director of Pharmacy Services, Fort Health Care
Listen to Podcast
Full Interview with Sarah Pagenkopf, Director of Pharmacy Services, and Tyler Prickette, Clinical Pharmacist at Fort HealthCare, including:
- getting buy-in from leadership to initiate opioid stewardship
- conducting a gap analysis
- identifying a champion leader
- setting goals and
- offering lessons learned and advice for pharmacist colleagues in rural settings
00:04:50
Listen to Audio Clip
How an opioid stewardship team at a rural Wisconsin health system got buy-in from leadership to initiate opioid stewardship projects
Clip from Podcast with Sarah Pagenkopf, Director of Pharmacy Services, Fort Health Care
00:44:37
Listen to Podcast
Full Interview with Sarah Pagenkopf, Director of Pharmacy Services, and Tyler Prickette, Clinical Pharmacist at Fort HealthCare, including:
- getting buy-in from leadership to initiate opioid stewardship
- conducting a gap analysis
- identifying a champion leader
- setting goals and
- offering lessons learned and advice for pharmacist colleagues in rural areas settings
How do I identify action leaders and champions for opioid stewardship?
 Identifying action leaders or champions for opioid stewardship who are willing to partner with the individual or small team initiating opioid stewardship is very important for obtaining buy-in from leadership as well as front frontline staff.
Identifying action leaders or champions for opioid stewardship who are willing to partner with the individual or small team initiating opioid stewardship is very important for obtaining buy-in from leadership as well as front frontline staff.
The Centers for Disease Control and Prevention (CDC) published a guide for implementing the 2016 CDC Guideline for Prescribing Opioids for Chronic Pain which included guidance related to opioid stewardship committees or task forces.
“Champions support and drive the change process, even in the face of organizational stagnancy, indifference, or active resistance. Effective champions in primary care settings are likely to possess leadership qualities even if they are not in leadership positions, are good models for others, and are skilled in motivating others to work as a team. They typically have strong relationships with leadership, which is an important resource when changes in established policies, approach, and workflow are needed. A champion should be someone on-site where the changes are taking place.” (CDC 2018)
The Society of Hospital Medicine (SHM) developed the Reducing Adverse Drug Events Related to Opioids (RADEO) Implementation Guide which provides step-by-step guidance to assist hospital teams in implementing a quality improvement program to improve patient safety and reduce opioid-related adverse events for patients receiving opioids.
The SMH guide recommends that the identified champion should be a well-respected individual (usually a provider) who is passionate about reducing opioid-related harms and who can promote the opioid stewardship efforts and convey why they are important for your health system. For example, they may advocate for the formation of opioid stewardship committee/task force. Module 4 offers additional guidance on this topic.
The champion will work alongside the person leading the opioid stewardship efforts and someone who is managing the project. Ideally, the person taking on the role of leading and/or managing opioid stewardship will have dedicated time to coordinate the day-to-day logistics (e.g., scheduling meetings, maintain communication, compile data, etc.) for moving the initiative along.
In rural healthcare settings, where clinicians often “wear many hats,” it is not uncommon for one person to be the champion, leader and project manager. This scenario can work well in small health systems, but it is important to ensure that the person taking on these roles has some amount of dedicated time to spend on opioid stewardship.
Steps for Identifying a Champion:
FIRST STEP: Compile a list of colleagues within the health system that possess the qualities of a successful champion. These include: possessing leadership qualities, being well-respected by colleagues, being passionate about opioid stewardship, being skilled at motivating others and being a good role model.
If you are unsure who these individuals are, consider existing committees within your health system that would likely have an interest in or be impacted by opioid stewardship. Examples include: Pharmacy and Therapeutics (P&T), Orthopedics, Emergency Medicine. This may have to be done repeatedly over time and across many committees.
SECOND STEP: Approach the identified colleagues individually to assess their interest in being a champion or ally for the opioid stewardship efforts.
How do I identify what my health system is already doing related to opioid stewardship?
Opioid stewardship encompasses a wide range of activities or initiatives related to optimal opioid prescribing for pain management, preventing adverse opioid-related events and treating harms related to opioids. Table 1 lists examples of opioid stewardship activities that health systems in Wisconsin have done in the recent past or are currently doing.
| Table 1. Examples of health system opioid stewardship activities | |||
| Appropriate opioid prescribing | Appropriate opioid disposal | Opioid diversion prevention | Managing opioid harms (e.g., treating opioid use disorder) |
|---|---|---|---|
| Implementing clinical decision support tools providing real-time alerts for high-risk patients. | Provide drop boxes for patients to dispose of unused opioids | Initiatives to prevent and deter employee diversion of opioids. | Encourage providers to prescribe naloxone for high-risk patients with opioid prescriptions |
| Engage with providers who have patients with high MME* prescriptions to explore opportunities for tapering patients to a lower dose | Coordinate with surrounding community to promote local drug take-back days | Order sets to encourage lower-risk opioids | Electronic health records functionality that automatically generates a naloxone prescription with every opioid prescription. |
*MME = morphine milligram equivalent
In some cases, there may be colleagues within a health system that are working independently on an opioid stewardship project or policy, which is not widely communicated across the health system. To compile a comprehensive list of what your health system is doing or has done, it is helpful to ask colleagues in different departments (e.g., emergency department, orthopedics, behavioral health) about whether they have worked on any opioid-related projects and policies. Provide them a brief definition of what you mean by opioid stewardship as defined in Module 1 and give them examples that would be relevant for their department or area of practice (Table 1).
The Centers for Disease Control and Prevention (CDC) published a guide for implementing the 2016 CDC Guideline for Prescribing Opioids for Chronic Pain which included about assessing current policies and practices.
 “Begin by assessing your current policies and practices for opioid prescribing.
“Begin by assessing your current policies and practices for opioid prescribing.
- Is your health system focused on maintaining accreditation with the Joint Commission or other bodies?
- Does your health system prioritize quality improvement?
- Is opioid stewardship consistent with your health system’s mission?
To more systematically assess current practices, your system could survey or interview clinicians about gaps in care or issues they encounter, or even ask questions at a staff meeting. You might also convene clinicians to discuss and reflect on key questions (e.g., “Do our current policies adequately address the issues that come up with patients on opioids?”). (CDC, 2018)
In addition to considering how opioid stewardship is being addressed within the health system, it’s important to conduct an environmental scan of the surrounding communities served by the health system.
An American Hospital Association 2020 publication focused on opioid stewardship measurement offers the following approach related to conducting an environmental scan to identify existing resources within the health system as well as in the surrounding community or county related to opioid stewardship.
- What services exist internally?
- What is the capacity to offer new services or improve/expand/enhance existing services?
- What services/initiatives exist within the community?
Module 8 has additional guidance about considering important stakeholders in the community and how their efforts are in alignment in your health system’s mission and goals.
Once you have taken stock of what you are already doing, you will be well-positioned to conduct a thorough needs assessment to identify where there are gaps related to opioid stewardship (see How do I conduct a needs assessment?).
How do I conduct a needs assessment?
Conducting a needs assessment or gap analysis will help to identify opioid stewardship areas that are not currently being addressed by your health system. Going through this process and documenting the opioid stewardship gaps will inform the discussions around setting priorities and goals related to opioid stewardship.
The Centers for Disease Control and Prevention (CDC) published a guide for implementing the 2016 CDC Guideline for Prescribing Opioids for Chronic Pain which included five steps for implementing an opioid stewardship effort.
Step 2. Assess Current Approaches for Opioids and Identify areas for Improvement
- Assess current policies and practices
- Complete the self-assessment questionnaire
- Collect data on your patient population and opioid therapy
- Determine access to specialists and other resources
- Identify areas to improve upon
Step 2 highlights the importance of assessing needs. Conducting a needs assessment often is an iterative process that may involve several rounds of revisions based on newly gathered information and input from providers and frontline staff across the organization. The small opioid stewardship team should put together a preliminary needs assessment based on their knowledge of what is already happening within their health system and identified gaps based on their knowledge of the best practices and recommendations. As the opioid stewardship team expands or there are opportunities for input from the leadership or administration, the needs assessment can be revised and refined.
There are some useful resources available to guide a needs assessment or gap analysis.
The Centers for Disease Control and Prevention (CDC) published a guide for implementing the 2016 CDC Guideline for Prescribing Opioids for Chronic Pain which included guidance related to conducting needs assessments.
It includes a Self-assessment Questionnaire for Health-Systems (pages 52-56) to use as a tool to assess to what extent the health system’s opioid stewardship practices are consistent with the CDC Guidelines.
The guide recommends that the questionnaire be completed by an individual who is leading the opioid stewardship efforts or by a team of individuals. Completion of the questionnaire can serve as a point of feedback if people have different assessments about the extent to which each step has been implemented or the extent to which clinicians are providing care consistent with the CDC Prescribing Guideline recommendations.
Part I “Status of Implementation Steps” is for the opioid stewardship team to reflect on and assess their health system’s status in progressing through the five steps to implementing for implementing the 2016 CDC Guideline for Prescribing Opioids for Chronic Pain.
Part 1 calls for indicating your health system’s current status with the tasks/activities within each of the five steps on a scale from 1 to 5, with 1 being you have not begun to 5 being you are done (for now). If the questionnaire is completed by multiple individuals, you can summarize the results by calculating an average for each of the steps in Part I. (CDC, 2018)
Examine the Data on Opioid Prescribing Trends to Identify Areas for Improvement
When responding to the items on the questionnaire, it may be necessary to collect basic patient population opioid-related data, for example:
- How many patients are on long-term opioid therapy?
- How many patients are prescribed opioids?
Your electronic health record (EHR) may have reports that you can run related to this information or you may have to collaborate with your IT colleagues to request a certain report. Module 5 of this toolkit has additional guidance about collecting data from your EHR and engaging with IT colleagues. The Wisconsin Prescription Drug Monitoring Program may also be a useful tool to identify patients and providers with prescribing that is considered at risk.
At this stage, you do not have to collect a large amount of data, but rather a sufficient amount of data to inform health system goals. These data can also be useful in preparing your rationale for the health system’s need for an opioid stewardship program. Compile data that shows where the health system is at currently and why they need to make a change. Use data to identify pockets of risk to target efforts where you can make a big difference to inform priorities and where to start.
00:03:31
Listen to Audio Clip
How an opioid stewardship team at a rural Wisconsin health conducted a needs assessment or gap analysis to identify areas of improvement
Clip from Podcast with Sarah Pagenkopf, Director of Pharmacy Services, Fort Health Care
Listen to Podcast
Full Interview with Sarah Pagenkopf, Director of Pharmacy Services, and Tyler Prickette, Clinical Pharmacist at Fort HealthCare, including:
- getting buy-in from leadership to initiate opioid stewardship
- conducting a gap analysis
- identifying a champion leader
- setting goals and
- offering lessons learned and advice for pharmacist colleagues in rural settings
How can my health system set realistic goals when first initiating opioid stewardship?
Based on your needs assessment results and the data gathered, the team will have identified areas for improvement in your policies, prescribing practices, workflows, and resources needed to support opioid stewardship. The assessment results might also bring to light the extent of unsafe practices with opioids (e.g., high dosages) in the health system.
Compile a comprehensive “wish list” of opioid-related improvement projects.
A first step may be to work with the team to compile a complete “wish list” of all the potential opioid-related improvement projects. Documenting these ideas may serve as the start of a long-range plan for an opioid stewardship program for the health system.
Prioritize the identified areas for improvement:
A second step is to review the list and organize the items by priority. Three criteria to consider when prioritizing the list of needed opioid stewardship activities are:
- Which changes are regarded as the most needed?
- Which changes would be the most effective at addressing the largest barriers?
- Which changes would be the most feasible or relatively simple to implement in the short-term to achieve an initial success, which will serve to build momentum for subsequent changes?
Pilot projects that can be implemented within 6 months help to sustain the momentum while allowing the bigger changes across the organization more time to come to fruition. Short-term wins through successful pilot projects provide the fuel needed to conquer resistance to practice change.
(Ghafoor et al., 2019)
The following are some examples of goals developed by a rural health system in Wisconsin.
Goals defined will evolve over time and should be continually revisited and revised. It is important to document the goals agreed upon by the opioid stewardship team.
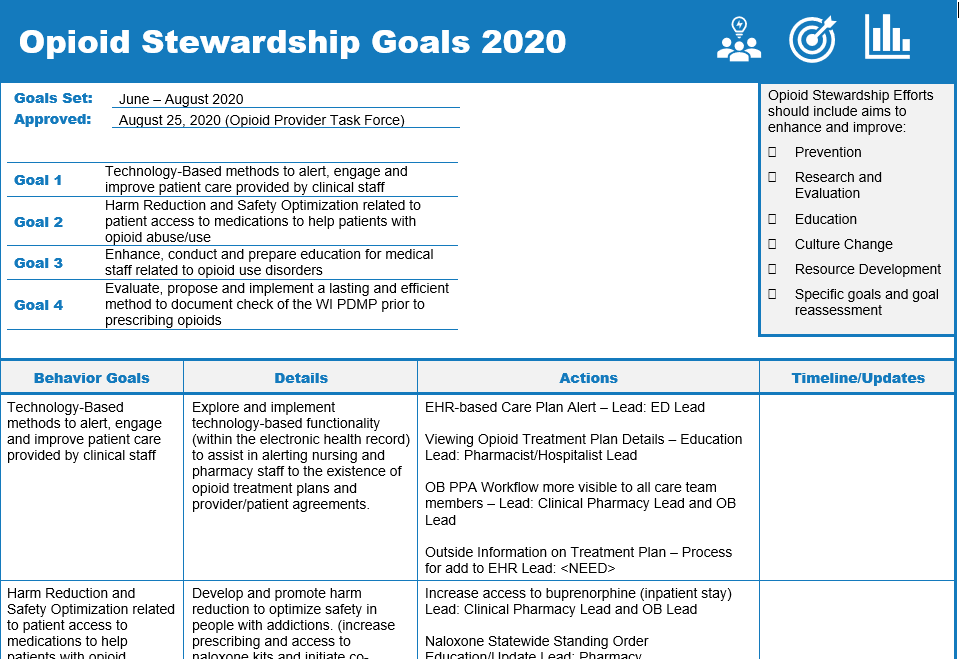 The goal-setting process and resulting framework can help unite members of the opioid stewardship team under common goals. Teams should be engaged to select goals that are specific, measurable, achievable, relevant to the larger goals of the team and time-bound (SMART). Outlining annual goals is a productive way to unite the team under a common plan, visualize the goals for the coming year, and offers a method to return to annual goals at each meeting, to check on progress, allow team members to provide updates, and to show action and results. This will help with team morale and cohesiveness. Fort HealthCare provided a template used by their teams to outline annual goals.
The goal-setting process and resulting framework can help unite members of the opioid stewardship team under common goals. Teams should be engaged to select goals that are specific, measurable, achievable, relevant to the larger goals of the team and time-bound (SMART). Outlining annual goals is a productive way to unite the team under a common plan, visualize the goals for the coming year, and offers a method to return to annual goals at each meeting, to check on progress, allow team members to provide updates, and to show action and results. This will help with team morale and cohesiveness. Fort HealthCare provided a template used by their teams to outline annual goals.
Download Sample Opioid Stewardship Goals (PDF)
00:03:31
Listen to Audio Clip
How a rural Wisconsin health system determined their highest priority goals when initiating opioid stewardship
Clip from Podcast with Sarah Pagenkopf, Director of Pharmacy Services, Fort Health Care
00:44:37
Listen to Podcast
Full Interview with Sarah Pagenkopf, Director of Pharmacy Services, and Tyler Prickette, Clinical Pharmacist at Fort HealthCare, including:
- getting buy-in from leadership to initiate opioid stewardship
- conducting a gap analysis
- identifying a champion leader
- setting goals and
- offering lessons learned and advice for pharmacist colleagues in rural settings
What is an example of a rural Wisconsin health system that obtained leadership buy-in to initiate opioid stewardship?
Listen to a podcast episode detailing an example of how a rural Wisconsin health system obtained leadership buy-in and initiated opioid stewardship.
Getting leadership buy-in and initiating opioid stewardship in a rural Wisconsin health system

Description:
- Interview with Sarah Pagenkopf, Director of Pharmacy Services, and Tyler Prickette, Clinical Pharmacist at Fort HealthCare, including:
- getting buy-in from leadership to initiate opioid stewardship
- conducting a needs assessment/gap analysis
- identifying a champion leader
- setting goals and
- offering lessons learned and advice for pharmacist colleagues in rural areas settings