This is an accordion element with a series of buttons that open and close related content panels.
How are health systems in a unique position to significantly contribute to addressing the opioid crisis?
The underlying principles of opioid stewardship – to optimize the quality of health care (i.e., pain management) and prevent adverse events (i.e., opioid harms) – are often aligned with health system missions to provide the best care and contribute to the health of the community. There are a number of reasons why health systems should prioritize opioid stewardship.
Health systems, including hospitals and outpatient clinics, play a significant role in prescribing opioids as a part of post-surgical care, orthopedics and through emergency departments. Given this, health systems have an opportunity to influence their providers’ prescribing behaviors and promote appropriate opioid prescribing. Individuals who overdose on opioids or experience opioid use disorder complications often present at the hospital for treatment, representing a critical opportunity to connect these individuals with potential treatment options. (Weiner et al., 2019)
“Providers and the health systems they work in are crucial in promoting safer and more effective opioid prescribing for pain management.”
What have national medical, scientific, and public health leaders said about health systems and opioid stewardship?
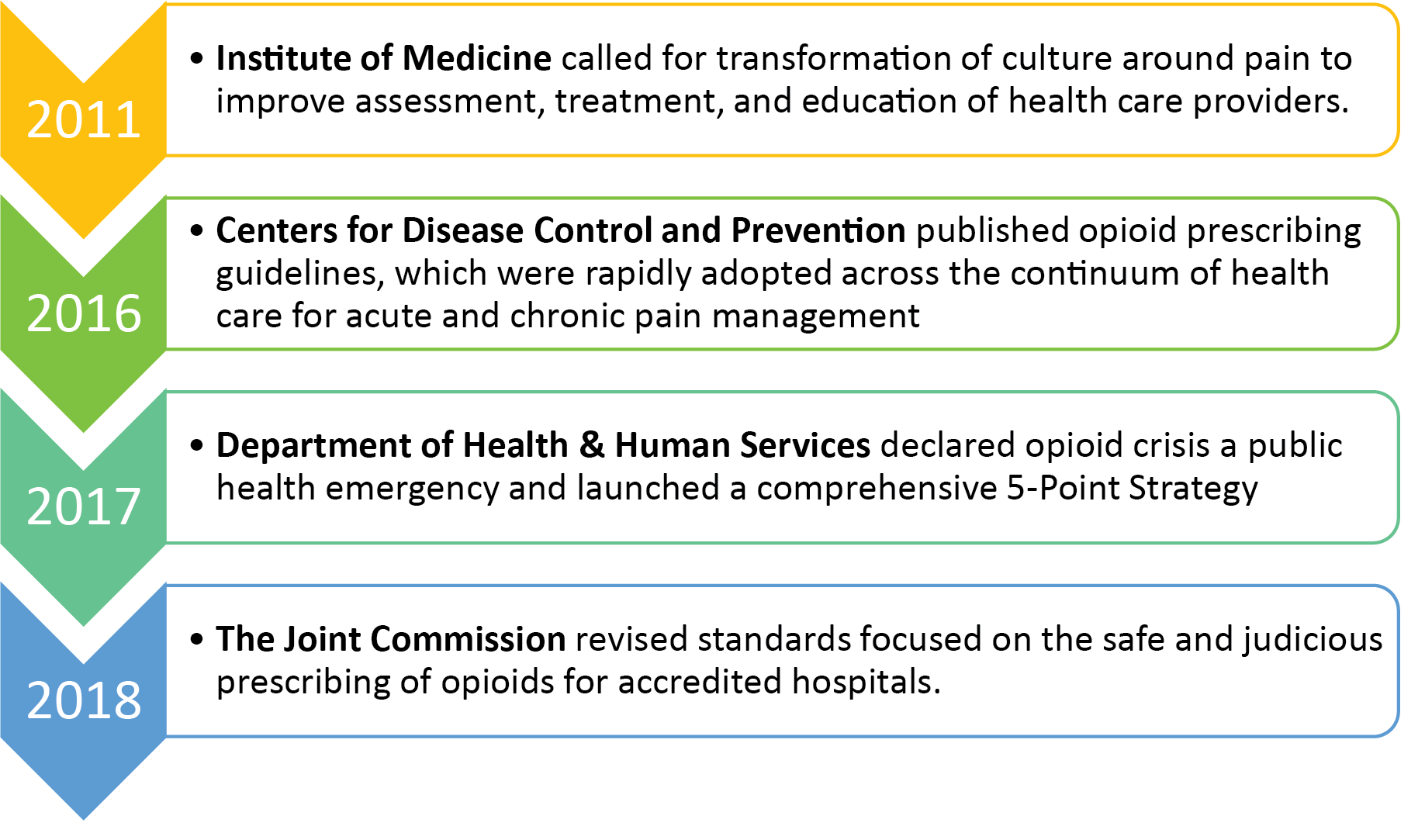
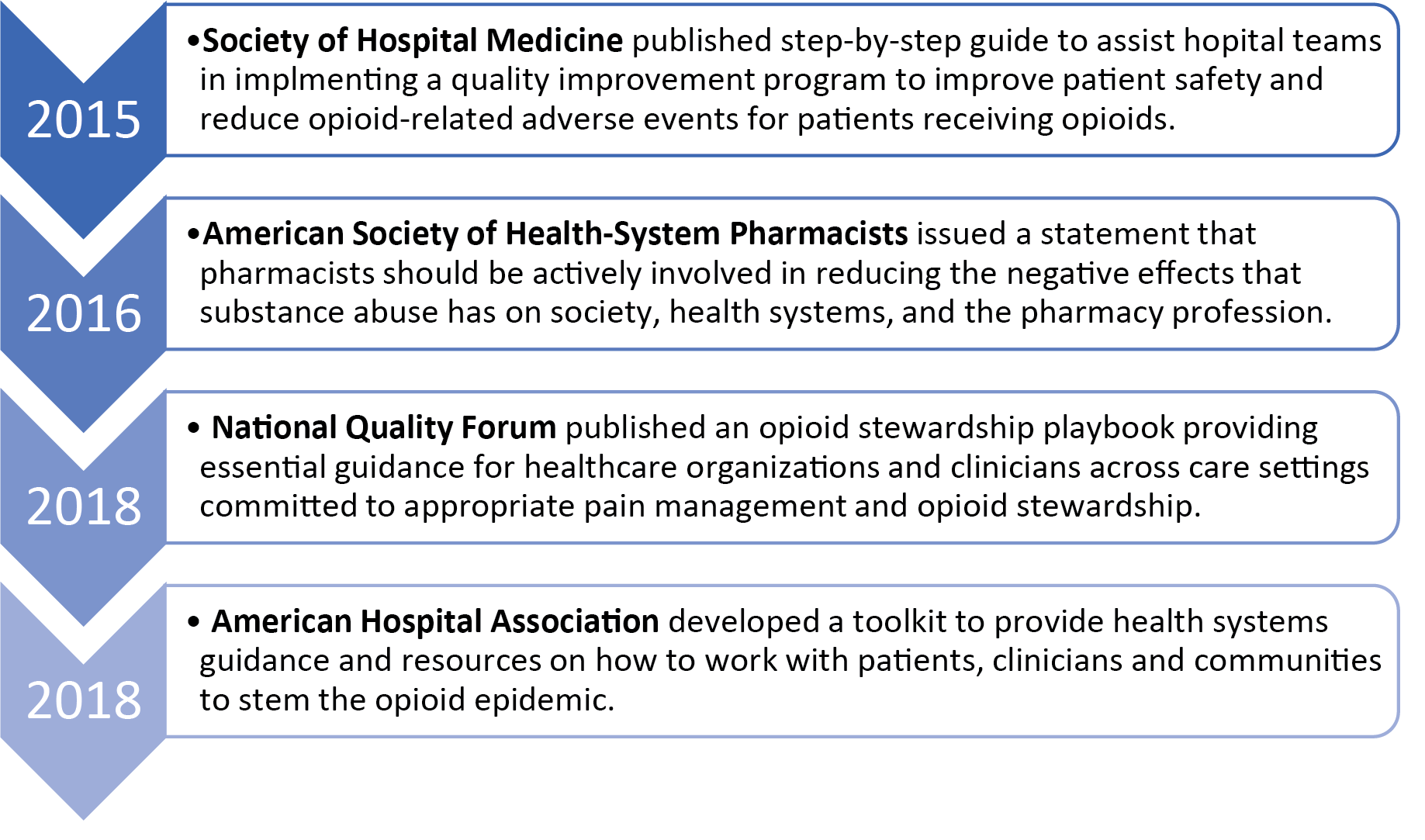
National & state medical, scientific, and public health leaders strongly recommend opioid stewardship efforts as a best practice for health systems. Numerous authoritative medical, scientific, and public health bodies strongly recommend/require/promote opioid stewardship. Below are some highlights of these statements and guidance. For a complete listing, download a PDF compilation of these policies, standards, guidelines, and resources with links to more information.
Medical and pharmacy professional organizations promoted opioid stewardship by issuing statements and resources to assist with implementing the best practices.
In Wisconsin, in 2019, the Wisconsin Medical Examining Board (MEB) issued an updated Opioid Prescribing Guideline with the purpose of helping providers make informed decisions about acute and chronic pain treatment (i.e., pain lasting longer than three months or past the time of normal tissue healing).
The guideline encourages providers to implement best practices for responsible prescribing which includes prescribing the lowest effective dose for the shortest possible duration for post-operative care and acutely-injured patients. Currently, there are no corresponding guidelines about opioids from the Wisconsin Pharmacy Examining Board. However, pharmacists can refer to the MEB guideline when presenting to health system leadership about the rationale for opioid stewardship.
In 2019, there was a new rule approved by the Wisconsin MEB requiring physicians with a DEA number to complete two CME credits on its Opioid Prescribing Guideline during each CME cycle. Currently, there is not a corresponding rule for pharmacists to complete CE in pain management or opioid-related topics, but pharmacy teams can refer to this requirement when presenting to health system leadership about the rationale for opioid stewardship and the role they can potentially play in pharmacist-delivered provider education.
How can opioid stewardship improve the assessment of health systems by federal quality and accountability programs evaluate?
Federal quality and accountability programs evaluate health systems based on meeting certain opioid stewardship milestones or opioid-related metrics. It is important for health systems and hospitals to meet national quality standards for opioid stewardship and to be in compliance with opioid-related reporting requirements developed by payers. Obtaining and renewing accreditation by national quality improvement bodies is important for hospitals and health systems to demonstrate their attainment and commitment to national quality standards. Similarly, health systems must report opioid-related health care quality measures to be eligible for certain reimbursements. Notably, as of 2019, the National Quality Forum (NQF) had identified over 200 health care quality measures related to pain management.
The Joint Commission
The Joint Commission is an independent, not-for-profit organization and is the nation’s oldest and largest standards-setting and accrediting body in health care, which accredits and certifies more than 22,000 health care organizations and programs in the United States, including hospitals and health care organizations.
Obtaining and renewing accreditation by the Joint Commission is important for hospitals and health systems to demonstrate their attainment and commitment to national quality standards.
In 2018, the Joint Commission released new and revised Pain Assessment and Management Standards for accredited hospitals. These standards included implementing policies and procedures for tracking and analyzing opioid incidents for quality improvement purposes, utilizing technology to monitor opioid prescribing, providing appropriate education and training of staff, and providing standardized tools to screen patients for risk factors associated with respiratory depression.
On January 1, 2019, new and revised Joint Commission pain assessment and management standards went into effect for accredited ambulatory care facilities and critical access hospitals.
These standards provide a framework and requirements that health systems need to meet to become accredited or renew their accreditation.
New requirements included:
- Identifying a leader or leadership team that is responsible for pain management and safe opioid prescribing
- Involving patients in developing their treatment plans and setting realistic expectations and measurable goals
- Promoting safe opioid use by identifying high-risk patients
- Monitoring high-risk patients
- Facilitating clinician access to prescription drug monitoring program databases
- Conducting performance improvement activities focusing on pain assessment and management to increase safety and quality for patients
The Joint Commission requires/recommends several specific opioid-related process and outcome measures, including:
| Table 1. Examples of Joint Commission opioid-related measures | |
| Domain | Measure |
|---|---|
| Acute Pain | Average Morphine Milligram Equivalent dose administered per inpatient day |
| Patient pain management planning and education | |
| Harm Reduction | Proportion of hospitalized patients administered naloxone |
| Number of adverse safety events due to opioids | |
| Identification and Treatment of Opioid Use Disorder (OUD) | Number of referrals for OUD / Medications for OUD |
| Completed/successful referrals for OUD treatment | |
Centers for Medicare and Medicaid Services (CMS)
As one of the largest payers for health care in the nation, CMS plays a critical role in addressing the opioid crisis and has incorporated opioid-related measures and improvement activities into several programs as detailed in Table 2.
| Table 2. Example of CMS Opioid-related measures across different programs | ||||
| Opioid-related measure or improvement activity | Merit Based Incentive Payment System (MIPS) Quality Measure or Improvement Activity | Medicaid Adult Core Set (ACS) | Medicare Shared Savings Program (MSSP) | Hospital Inpatient Quality Reporting Program (HIQRP) |
|---|---|---|---|---|
| Average total MME* per prescription | √ | √ | ||
| MME* per opioid prescription | √ | √ | ||
| Patient pain management planning and education | √ | |||
| Percentage of patients with opioids and benzodiazepines co-prescribed | √ | √ | √ | |
| Opioid prescriptions >90 MMEs* daily | √ | |||
| Proportion of hospitalized patients administered naloxone | √ | |||
| Opioid/controlled substance agreement signed | √ | |||
| New patient starts for Medications for Opioid Use Disorder (MOUD) | √ | |||
| Screening for Opioid Use Disorder /Substance Use Disorder | √ | |||
*MME = Morphine Milligram Equivalent
Healthcare Effectiveness Data and Information Set (HEDIS) measures – National Committee for Quality Assurance
Beginning in the early 1990s, the National Committee for Quality Assurance is a national leader in measuring performance in health care and accrediting health plans. They have been hired by government and private sector organizations to assist with measuring and improving quality. Nearly 200 million people are enrolled in health plans that report HEDIS results, making HEDIS measures one of the most common quality improvement tools.
The HEDIS measures include over 90 measures across 6 domains of care.
- Effectiveness of Care
- Access/Availability of Care
- Experience of Care
- Utilization and Risk Adjusted Utilization
- Health Plan Descriptive Information
- Measures Reported Using Electronic Clinical Data Systems
Table 3 lists examples of HEDIS measures related to opioid stewardship.
| Table 3. Examples of HEDIS measures related to opioid stewardship | |
| Measure | Description |
|---|---|
| Use of Opioids at High Dosages (HDO) | Assesses potentially high-risk opioid analgesic prescribing practices: The proportion of members 18 years and older who received prescription opioids at a high dosage (average morphine milligram equivalent dose [MME] ≥90) for ≥15 days during the measurement year. |
| Use of Opioids from Multiple Providers (UOP) | Assesses potentially high-risk opioid analgesic prescribing practices: The proportion of members 18 years and older, receiving prescription opioids for ≥15 days during the measurement year from multiple providers. Three rates are reported.
|
| Risk of Continued Opioid Use (COU) | Assesses potentially high-risk opioid analgesic prescribing practices: The percentage of members 18 years and older who have a new episode of opioid use that puts them at risk for continued opioid use. Two rates are reported:
|
How will health system opioid stewardship initiatives linked with the surrounding community contribute to meeting the federal requirement that the health system is producing community benefits?
For nonprofit hospitals, establishing opioid stewardship initiatives linked with the surrounding community will contribute to meeting the federal requirement that the health system is producing community benefits with the costs saved from tax exemptions. Nearly 60% of all hospitals in the US are non-profit. In 2010, the Patient Protection and Affordable Care Act (ACA) added new requirements for non-profit hospitals to demonstrate that they were providing sufficient benefit to the community to rationalize their status as tax-exempt. All nonprofit hospitals were mandated to: (1) conduct a triennial community health needs assessment (CHNA) and adopt an implementation strategy, (2) abide by specific documentation requirements, and (3) make these documents publicly available. Failure to fulfil these requirements could jeopardize a nonprofit hospital’s ability to receive tax exemptions.
The opioid crisis is multifaceted and affects communities served by health systems. By prioritizing opioid stewardship, health systems are contributing to addressing the opioid crisis across the communities they serve. Health systems can include their opioid stewardship initiatives in their community health needs assessments to contribute to the justification of their tax-exempt status. Module 8 provides additional guidance about establishing health system partnerships with the community to optimize opioid stewardship efforts.
In what ways does opioid stewardship contribute to optimizing population health and align with health system missions to promote health across the community?
 Opioid stewardship is necessary for optimizing population health and aligns with health system missions to promote health across the community. The opioid epidemic is a national public health crisis affecting nearly all communities, including rural communities. It is multifaceted and affects many aspects of communities including, emergency departments, operating rooms, neonatal intensive care units, police, fire, EMT, family practice, behavioral health, dental, pharmacies, and schools. Health system opioid stewardship efforts contribute to population health by addressing the opioid crisis throughout the communities served by the health system. Often this population health-focused approach is in alignment with the health system’s mission and goals to create a healthy community. Health system opioid stewardship initiatives may not be revenue-generating, but rather they are critically needed to address a national public health crisis that is impacting all communities. There are many potential non-monetary benefits to implementing opioid stewardship, such as improvements in safety, efficiency, reducing readmissions, return to office or emergency room visits. It is important to think outside of the box about how the value of opioid stewardship to the health system is defined.
Opioid stewardship is necessary for optimizing population health and aligns with health system missions to promote health across the community. The opioid epidemic is a national public health crisis affecting nearly all communities, including rural communities. It is multifaceted and affects many aspects of communities including, emergency departments, operating rooms, neonatal intensive care units, police, fire, EMT, family practice, behavioral health, dental, pharmacies, and schools. Health system opioid stewardship efforts contribute to population health by addressing the opioid crisis throughout the communities served by the health system. Often this population health-focused approach is in alignment with the health system’s mission and goals to create a healthy community. Health system opioid stewardship initiatives may not be revenue-generating, but rather they are critically needed to address a national public health crisis that is impacting all communities. There are many potential non-monetary benefits to implementing opioid stewardship, such as improvements in safety, efficiency, reducing readmissions, return to office or emergency room visits. It is important to think outside of the box about how the value of opioid stewardship to the health system is defined.