This is an accordion element with a series of buttons that open and close related content panels.
What is the US opioid crisis?
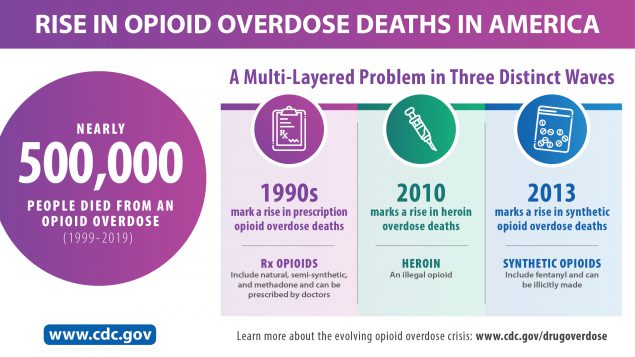 The opioid crisis, including prescription opioid misuse, abuse, and associated overdose deaths, represents a decades-long major public health issue. The Centers for Disease Control and Prevention (CDC) reported that between 1999–2019, approximately 500,000 people died from opioid-related overdose.
The opioid crisis, including prescription opioid misuse, abuse, and associated overdose deaths, represents a decades-long major public health issue. The Centers for Disease Control and Prevention (CDC) reported that between 1999–2019, approximately 500,000 people died from opioid-related overdose.
The U.S. Department of Health and Human Services cited key opioid epidemic statistics from 2019 data:
- 10.1 million people misused prescription opioids in the past year
- 48,006 deaths attributed to overdosing on synthetic opioids other than methadone from June 2019-June 2020
- 1.6 million people had an opioid use disorder in the past year.
The CDC has found that since 2020, the opioid crisis has been further exacerbated by COVID-19 pandemic-related treatment disruptions, increased isolation and mental health needs. Preliminary CDC data from 2020 indicate there were an estimated 93,331 drug overdose related deaths of which 69,769 involved opioids. This represents an all-time high.
The US Centers for Disease Control and Prevention and others classify the opioid crisis into three waves of opioid overdose deaths:
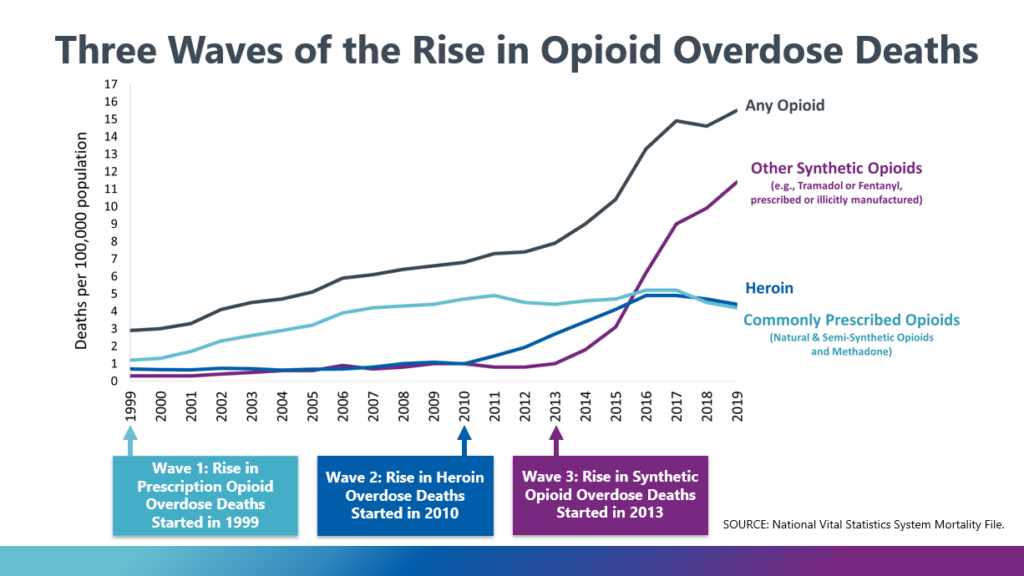
- Increased prescribing of opioids in the 1990’s
- Beginning around 2010, a wave of overdose deaths involving heroin, and
- Around 2013 significant increase in overdose deaths involving synthetic opioids, including illicitly manufactured fentanyl.
Most recently, the US is experiencing a fourth wave of the opioid and substance use disorder crisis involving polysubstance use, specifically the co-use of opioids and psychostimulants such as methamphetamine, cocaine.
In 2017 the US Department of Health and Human Services declared a public health emergency and announced a 5-Point Strategy To Combat the Opioid Crisis.
How has the opioid crisis affected rural communities across the US?
 The opioid crisis has had dire effects on all communities across the US (i.e., urban, suburban and rural) regardless of size. However, rural communities, which frequently lack the services and substance use treatment facilities that are often more available in urban and suburban areas, have experienced dramatic increases in rates of opioid abuse and overdose.
The opioid crisis has had dire effects on all communities across the US (i.e., urban, suburban and rural) regardless of size. However, rural communities, which frequently lack the services and substance use treatment facilities that are often more available in urban and suburban areas, have experienced dramatic increases in rates of opioid abuse and overdose.
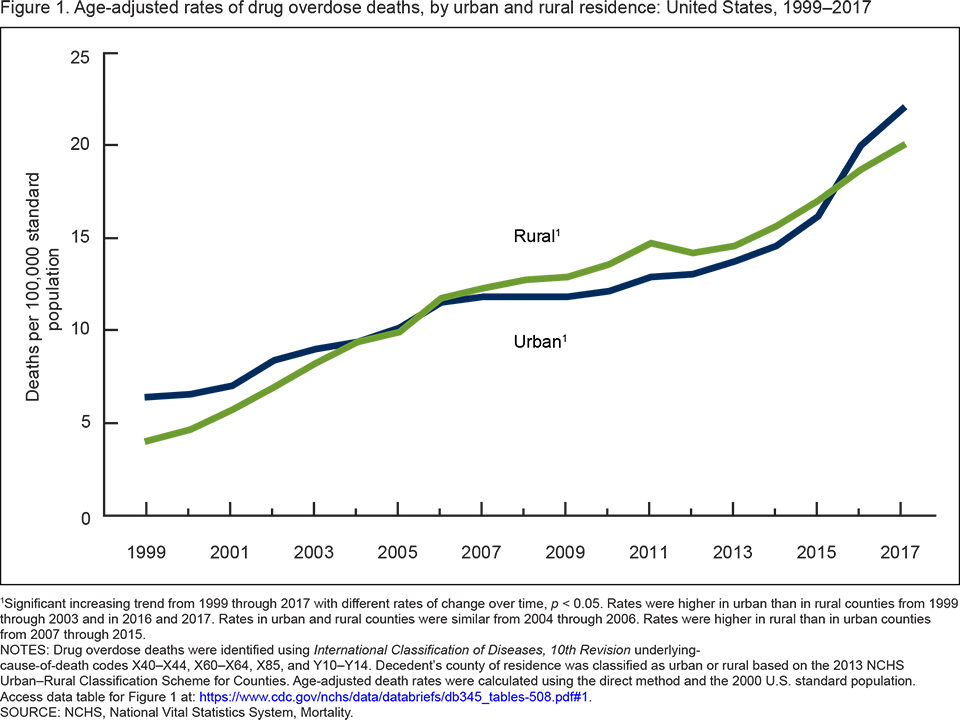
A 2019 CDC National Center for Health Statistics Data Brief reported that from 2007 to 2015, drug-overdose death rates were higher in rural than in urban counties, though around 2015, rates in urban areas surpassed rural areas.
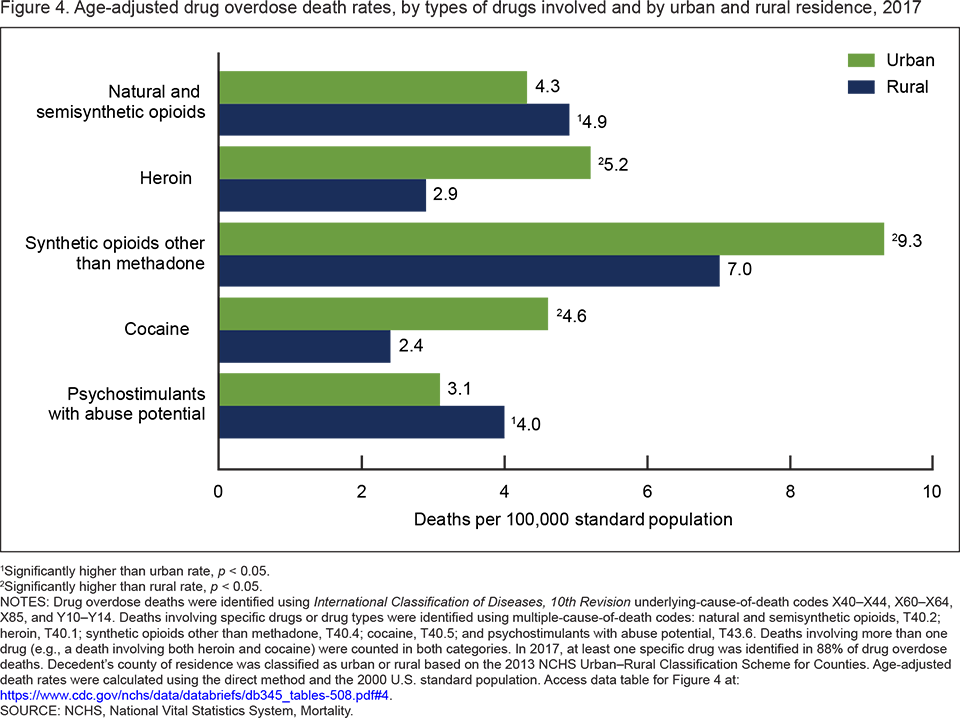
However, in 2017, the rates of drug overdose deaths for certain types of drugs including opioids were higher in rural areas than urban areas.
- In 2017, the rate of drug overdose deaths involving natural and semisynthetic opioids (e.g., oxycodone, hydrocodone, morphine, and codeine) was higher in rural (4.9 per 100,000) than in urban (4.3 per 100,000) counties.
- The rates of drug overdose deaths involving natural and semisynthetic opioids (e.g., morphine, codeine, hydrocodone oxycodone) and involving psychostimulants with abuse potential (e.g., methamphetamine) were higher in rural counties than in urban counties. (NCHS Data Brief, No. 345, August 2019)
Rural communities across the US experience many inequities compared to urban and suburban areas. Rural residents often have fewer individual resources and, on average, are poorer and less educated. (Rural Health Information Hub)
The Rural Health Information Hub Rural Prevention and Treatment of Substance Use Disorders Toolkit describes the many factors that contribute to the significant burden of opioid misuse and related harms in rural communities, including:
| High poverty and unemployment |
|
|---|---|
| Increased availability of prescription opioids |
|
| Barriers to treatment for opioid harms |
|
How has Wisconsin been impacted by the opioid crisis?
 Wisconsin has been hard-hit by the opioid crisis. The annual number of opioid overdose deaths have been increasing. There were over eleven times as many deaths in 2020 as in 2000.
Wisconsin has been hard-hit by the opioid crisis. The annual number of opioid overdose deaths have been increasing. There were over eleven times as many deaths in 2020 as in 2000.
And the annual number of opioid-related emergency room visits increased 310% from 2007 to 2020.
Data from the National Institute on Drug Abuse, 2018, indicate that Wisconsin continues to have higher rates of opioid-involved deaths and related harms compared with national rates.
In 2020, the Wisconsin Department of Health Services (DHS) released a report identifying areas of Wisconsin most in need of resources to prevent, intervene, and treat the harms of the opioid crisis.
The zip codes with rates in the highest 20% for any of the four indicators of opioid overdoses and infectious harms from drug use were identified as areas of concern.
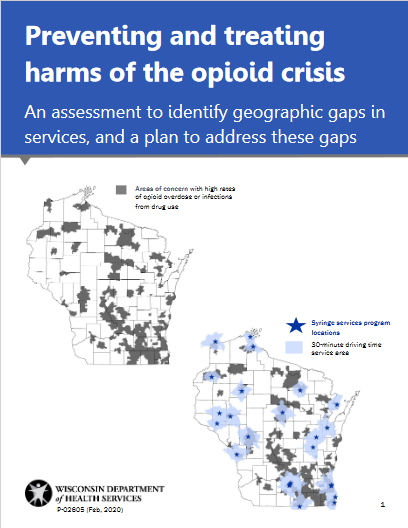
Next DHS mapped the location of prevention and treatment resources including buprenorphine providers, opioid treatment programs, and naloxone availability at pharmacies.
Maps were overlayed to identify the gaps where the prevention and treatment resources are most needed.
The results of the assessment will be used to inform the allocation of resources and to improve access to prevention and treatment resources in the areas of Wisconsin that need them the most.
However, data from the Wisconsin Prescription Drug Monitoring Program shows that there was a decline in the number of opioid prescriptions between 2016 and 2020.
How have rural areas of Wisconsin been impacted by the opioid crisis?
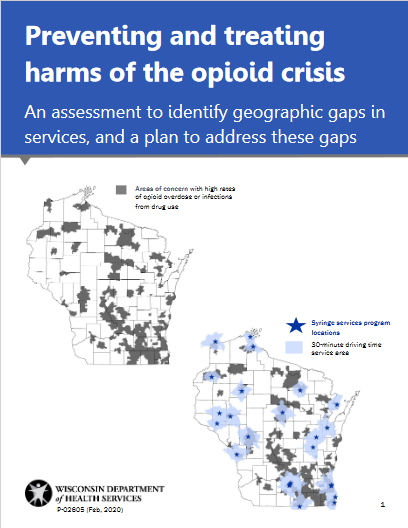
In 2020, the Wisconsin Department of Health Services (DHS) conducted a mapping assessment to identify areas of Wisconsin most in need of resources to prevent, intervene, and treat the harms of the opioid crisis. A report was released, Preventing and treating the harms of the opioid crisis: An assessment to identify geographic gaps in services, and a plan to address these gaps, with the findings.
The report identified areas of concern, particularly in more rural areas of Wisconsin, that are not within a reasonable driving distance of pharmacies with a standing order for naloxone, syringe services programs, medication-assisted treatment providers, substance use treatment providers, hepatitis C treatment providers, and HIV prevention services.
Rural Voices for Prosperity: A Report of the Governor’s Blue Ribbon Commission on Rural Propserity, highlighted the impacts the opioid crisis continues to have on rural Wisconsin.
Stakeholders also underline alcohol and drug abuse, including the addiction to opioids that has plagued the nation in recent years. These problems persist and are growing in rural areas, especially those that offer less opportunity to make a good living.”
The report acknowledges underlying issues related to accessing health care in rural areas, which includes the lack of resources to address the opioid crisis in rural areas.
“Access to health care services and facilities is in serious condition in much of rural Wisconsin. Stakeholders also raised deep concern about the lack of nearby health care professionals, care centers and rural hospitals. Indeed, though about 20% of Wisconsin’s population is rural, less than 10% of the state’s physicians practice in rural areas.”
What is Opioid Stewardship?
The American Hospital Association (AHA) defines opioid stewardship as:
AHA characterized opioid stewardship programs as:
A key characteristic of opioid stewardship programs is that they are systematic and provide a framework for a hospital or health system to identify areas in need of quality improvement related to opioids and implement changes in institutional culture and practice to improve the judicious use of opioids. Additionally, opioid stewardship programs involve the formation of multidisciplinary teams of providers and frontline staff working together on managing opioids, which in turn, helps to shift the burden for managing opioid prescribing from individual providers.
The concept of opioid stewardship is modeled on antimicrobial stewardship which emerged in the late 1990s in response to a rise in unnecessary antibiotic use and increasing antibiotic resistance. The Centers for Disease Control and Prevention (CDC) promotes antimicrobial stewardship in “…helping prescribers use the right antibiotic, at the right dose, for the right duration, and at the right time, and reduce unnecessary antibiotic use.”
Similarly, the need for opioid stewardship programs emerged as a response to the opioid crisis. The National Quality Forum (NQF) is a not-for-profit, nonpartisan, membership-based organization that provides measures and standards that serve as a critically important foundation for initiatives to enhance healthcare value and patient safety. NQF developed the gold standard recommendations for antimicrobial stewardship and in 2017 built on this work to develop similar guidance for opioid stewardship, National Quality Partners Playbook: Opioid Stewardship.
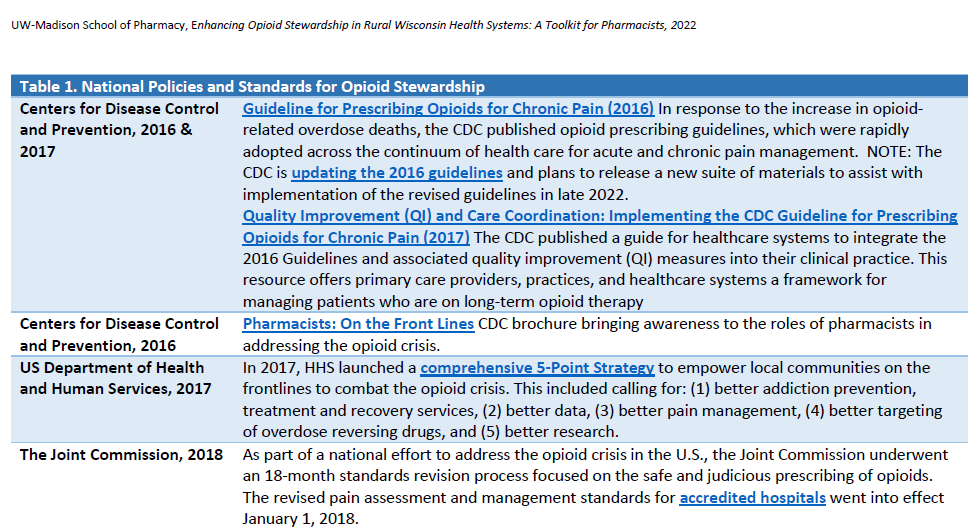
The concept of opioid stewardship is rooted in several recommendations for pain management from national medical, scientific and public health authorities (Table 1).
| Table 1. Origins of Opioid Stewardship | |
| Institute of Medicine Committee on Advancing Pain Research, Care, and Education, 2011 |
Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research The US Department of Health and Human Services, National Institutes of Health, requested that the Institute of Medicine convene an ad hoc committee to address the state of the science with respect to pain research, care, and education; and explore approaches to advance the field. The resulting report called for the transformation of the culture around pain to improve assessment, treatment, and education of health care providers. |
|---|---|
| Centers for Disease Control and Prevention, 2016 & 2017 | Guideline for Prescribing Opioids for Chronic Pain (2016) In response to the increase in opioid-related overdose deaths, the CDC published opioid prescribing guidelines, which were rapidly adopted across the continuum of health care for acute and chronic pain management. NOTE: The CDC is updating the 2016 guidelines and plans to release a new suite of materials to assist with implementation of the revised guidelines in late 2022.Quality Improvement (QI) and Care Coordination: Implementing the CDC Guideline for Prescribing Opioids for Chronic Pain (2017) The CDC published a guide for healthcare systems to integrate the 2016 Guidelines and associated quality improvement (QI) measures into their clinical practice. This resource offers primary care providers, practices, and healthcare systems a framework for managing patients who are on long-term opioid therapy. |
| National Quality Forum, 2018 | The National Quality Forum (NQF) convened an Opioid Stewardship Action Team in 2017, which included 40+ organizations representing clinicians, patient partners, federal agencies, and other key stakeholders. In 2018, the NQF published the NQP Playbook™: Opioid Stewardship, which provides essential guidance for healthcare organizations and clinicians across care settings committed to appropriate pain management strategies and opioid stewardship. |
| The Joint Commission, 2018 & 2019 |
Effective Jan. 1, 2018, the Joint Commission released new and revised Pain Assessment and Management Standards for accredited hospitals. These standards included implementing policies and procedures for tracking and analyzing opioid incidents for quality improvement purposes, utilizing technology to monitor opioid prescribing, providing appropriate education and training of staff, and providing standardized tools to screen patients for risk factors associated with respiratory depression.
On January 1, 2019, new and revised Joint Commission pain assessment and management standards went into effect for accredited ambulatory care facilities and critical access hospitals. |
Opioid stewardship activities or programs encompass many different activities related to improving the judicious use of opioids related to prescribing, disposal, diversion prevention and managing harms. Table 2 lists examples of opioid stewardship activities.
| Table 2. Examples of Health System Opioid Stewardship Activities | |||
| Appropriate opioid prescribing | Appropriate opioid disposal | Opioid diversion prevention |
Managing opioid harms (e.g., treating opioid use disorder) |
|---|---|---|---|
| Implementing clinical decision support tools providing real-time alerts for high-risk patients. | Provide drop boxes for patients to dispose of unused opioids | Initiatives to prevent and deter employee diversion of opioids. | Encourage providers to prescribe naloxone for high-risk patients with opioid prescriptions |
| Engage with providers who have patients with high MME* prescriptions to explore opportunities for tapering patients to a lower dose | Coordinate with surrounding community to promote local drug take-back days | Order sets to encourage lower-risk opioids | Electronic health records functionality that automatically generates a naloxone prescription with every opioid prescription. |
*MME = morphine milligram equivalent
It is important to note that the process of developing opioid stewardship has many components and can take time. Oftentimes the process is not linear, but iterative, requiring teams to continuously revisit decisions, plans and goals to assess whether they need to be modified.
Each module of this toolkit explores a different opioid stewardship topic, including:
- Module 2: Prioritizing Opioid Stewardship
- Module 3: Getting Leadership Buy-In
- Module 4: Forming Leadership Teams
- Module 5: Using Electronic Health Record (EHR) Data to Measure Outcomes
- Module 6: Enhancing Pharmacist Roles
- Module 7: Educating about Opioid Stewardship
- Module 8: Establishing Partnerships with Community
This 2019 article highlights a 17-year effort (led by pharmacists) to implement an opioid stewardship program in a health system in Minnesota.
Listen to Audio Clip
Examples of opioid stewardship activities at a rural Wisconsin health system
Clip from Podcast with Sarah Pagenkopf, Director of Pharmacy Services, Fort Health Care
00:44:37
Listen to Podcast
Full Interview with Sarah Pagenkopf, Director of Pharmacy Services, and Tyler Prickette, Clinical Pharmacist, from Fort Health Care including:
- getting buy-in from leadership to initiate opioid stewardship
- conducting a gap analysis
- identifying a champion leader
- setting goals and
- offering lessons learned and advice for pharmacist colleagues in rural areas settings
What are the policies, standards, and best practices for opioid stewardship?
 There are numerous policies, standards, and best practices for opioid stewardship from national and Wisconsin state public health, quality improvement and professional pharmacy organizations. In addition, there are valuable resources to assist health system teams in implementing opioid stewardship. Download a PDF compilation of these policies and standards including links to more information.
There are numerous policies, standards, and best practices for opioid stewardship from national and Wisconsin state public health, quality improvement and professional pharmacy organizations. In addition, there are valuable resources to assist health system teams in implementing opioid stewardship. Download a PDF compilation of these policies and standards including links to more information.