7
December

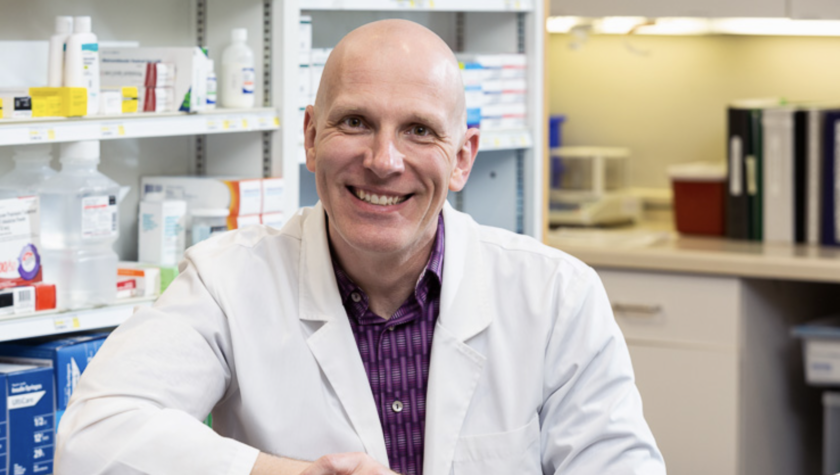
Streu’s Pharmacy in Green Bay provides much-needed medication-assisted therapy for opioid and alcohol misuse
By Katie Ginder-Vogel
Up to 65 percent of incarcerated individuals have a substance use disorder. When released from prison, they often return to their vices and experience high rates of overdose, even fatal overdoses, within the first few months.
One of the missing links connecting recently released inmates to a new, clean life is a lack of access to treatment centers, which are especially rare in rural communities. A recent analysis by Kevin Look, assistant professor in the University of Wisconsin–Madison School of Pharmacy’s Social and Administrative Sciences Division, found that community pharmacies are essential in addressing the glaring shortage of formal treatment centers: All but one of Wisconsin’s 14 rural counties without a formal treatment facility had at least one community pharmacy.
“There is an unmet need in the community for medication-assisted therapy,” says John Lemke (PharmD’ 15), a pharmacist at Streu’s Pharmacy Bay Natural in Green Bay, Wisconsin. “You don’t have to look very far to see the devastating effects of opioid and alcohol abuse.”
Pharmacists in Wisconsin have only recently been permitted by law to provide non-vaccine medication injections. Act 290, passed in 2015, expanded pharmacists’ role to include delivering injections of naltrexone (a long-acting opiate antagonist also used to discourage alcohol abuse) and long-acting antipsychotics.
“Empowering pharmacists to provide these injections is a way to address the dearth of behavioral health providers and addiction treatment facilities in Wisconsin.”
—John Lemke
Since the passage of Act 290, Lemke and Streu’s owner Jeff Kirchner (BS ’88) began offering injections in 2016 and forged a partnership with the Manitowoc County Human Services Department in 2017 to help inmates in the county’s correctional system access ongoing naltrexone treatment for opioid misuse disorder and alcoholism following their release. In doing so, Streu’s became one of the first pharmacies in Northwest Wisconsin to offer these injections. Now, there are 13 injection providers in a 50-mile radius of Green Bay, several of which are pharmacies, including Luxemburg and Hometown Pharmacies.
“Empowering pharmacists to provide these injections is a way to address the dearth of behavioral health providers and addiction treatment facilities in Wisconsin, particularly in rural areas,” says Lemke. “The populations who need these two services often overlap.”
As medication-assisted therapy has steadily grown to meet an urgent need in rural communities, Streu’s partnerships have also expanded to include the Brown County Department of Corrections, with other promising collaborations in the works.
But, even after the passage of Act 290, there are still more roadblocks that persist for pharmacists hoping to sustainably implement the service.
Launching a naltrexone program
As Lemke and Kirchner were considering offering medication-assisted therapy at Streu’s, Alay Health Team, a psychiatric clinic, approached Streu’s during their search for injection locations in Wisconsin, particularly in rural areas. Then Lemke learned that the Manitowoc County Department of Corrections was seeking partners to offer naltrexone injection services, as well.

“It became obvious we should become an injection service provider,” says Lemke. “We initiated the naltrexone program in December of 2016 as a private partnership with group of nurse practitioners from Alay Health Team and saw our first patient in January of 2017.”
That first year, they saw just one or two patients, but each year since, they’ve gained momentum and established more county-level connections.
As Streu’s naltrexone program approaches its three-year anniversary, the pharmacy’s partnership with the Manitowoc County, which is run through in collaboration with the county’s inmate transition program, continues. Streu’s has begun working with the Brown County Department of Health Services and the Alcohol and Other Drug Abuse Programs (AODA) of the Wisconsin Department of Health Services (DHS) and is developing their process for working with the Wisconsin Department of Corrections. In addition, Lemke recently presented information about naltrexone and Streu’s injection services to assessors from DHS’s Impaired Drivers Program.
“Once we started working with Brown County and AODA, we got more patients via county, patient, and provider referral,” says Lemke. “Now, as referrals are growing, we treat about 15 patients a month, and there is a wide network of doctors who prescribe medication-assisted therapy.”
Providing accessible, flexible care
Streu’s approaches referrals like clinical appointments, and Streu’s employees reach out to patients as soon as a new referral comes in.
“We can act very quickly,” says Lemke. “One patient was at the doctor’s office and presented as ready to be treated that day and in danger of using that day if they couldn’t be treated. We were able to coordinate with the doctor’s office to get that patient in immediately.”
Streu’s Pharmacy has multiple pharmacists and nurses on staff who are trained to administer injections and are available at odd hours and on weekends. Coordination can happen on the fly, or patients can set up an appointment.
“When they arrive, they sit down with a pharmacist in our clinical waiting room,” says Lemke. The pharmacist educates the patient and administers a private injection, and then patients receive follow-up calls and reminders to return for monthly injections, including calls for missed appointments.
“Medication-assisted therapy offers benefits,” says Lemke. “There is a decent rate of recidivism, but for every one of those cases, there’s someone else who comes on time for their injection every month for the full year of treatment and comes back to thank us later.”
Lemke says he’s received hugs and cards from patients who are grateful to have their lives back.
“The rewarding part is that this is making a difference; addiction treatment is actual life or death stuff,” Lemke says. “It’s fulfilling, impactful, and the more we can do to make treatment related to the opioid crisis available, the better for us and our community.”
Lingering roadblocks
While care providers often work in silos — the courts, county behavioral health departments, primary care offices, recovery coaches, counselors, and emergency rooms — Lemke says pharmacists are uniquely positioned to work across boundaries to provide quick care. But some remaining legal obstacles remain, limiting pharmacists’ ability to help.
“If there are barriers where you can’t coordinate care, patients suffer,” says Lemke. “I’ve seen enough people hit roadblocks with their insurance companies, and 24 hours can be the difference between staying clean and using again. Every second we wait is a chance someone has to relapse.”

Typically, a recently released inmate in need of medication-assisted therapy for opioid misuse disorder or alcoholism moves to a halfway house after being released, and the halfway house provides transportation to the pharmacy for the first injection. However, a complicated reimbursement structure makes it difficult for halfway houses to guarantee patient transportation for ongoing treatment. Fortunately, as more pharmacies become injection sites, the transportation barrier is getting lower.
Another barrier is that over half of the patients referred to Streu’s and other pharmacies are using Medicaid to pay for the treatment. Pharmacists, although they have provider status in Wisconsin, are not considered providers by Medicaid, so they can’t get reimbursed for the injection services they provide — only the drug itself, which costs about $1,300.
Pharmacists aren’t compensated for administering the injection, or the time and resources that go into managing the patient, such as conducting drug tests, scheduling injections, educating patients, and following up.
“There’s no billing pathway,” says Lemke. “We can bill for giving a flu shot, which takes moments, but naltrexone appointments take 15 minutes minimum.”
“The rewarding part is that this is making a difference; addiction treatment is actual life or death stuff.”
—John Lemke
Lemke says the lack of reimbursement holds many pharmacists back from providing injection services, especially in the rural areas that need them most. But because of the benefits each injection holds for the community, Streu’s continues to provide the service, at a loss, while working to change the reimbursement structure.
“We are working with state Medicaid, gathering our own cost data, and talking to legislators to get paid for our professional services, which provide an unmet need in the marketplace and help patients in a convenient, non-stigmatizing way,” says Lemke. “This drug has a high price tag, so we’re just asking for fair compensation.”
Pharmacists provide much-needed access to medication-assisted therapy, which positively impacts communities around Wisconsin and the country. These vital services illuminate the importance of pharmacists being fairly reimbursed and recognized for the care they provide.
“Physicians are on board; lawmakers are on board; other folks in community levels of government all want this to be successful for patients and to figure out a model to reimburse pharmacists,” Lemke says. “The buy-in is there. Everyone wants medication-assisted therapy to be successful.”