By Eric Hamilton
This article originally appeared on UW–Madison’s news page.
University of Wisconsin–Madison researchers have developed nanoparticles that, in the lab, can activate immune responses to cancer cells. If they are shown to work as well in the body as they do in the lab, the nanoparticles might provide an effective and more affordable way to fight cancer.
They are cheaper to produce and easier to engineer than the antibodies that underlie current immunotherapies, which as drugs cost tens of thousands of dollars a month.
“Immunotherapy basically boosts the patient’s own immune system to fight against cancer cells better,” says Seungpyo Hong, a professor in the UW–Madison School of Pharmacy. “The antibodies that are used right now are large, they’re expensive, they’re hard to engineer, and they don’t always show the highest level of efficacy either. So we wanted to explore other ways to activate the immune system.”
Hong and postdoctoral associate Woo-jin Jeong led the study, published online Jan. 2 in the Journal of the American Chemical Society, with collaborators at the University of Illinois at Chicago. It’s the first demonstration that nanoparticles can act as immunotherapy agents.
More research is needed to understand their effectiveness in the body, but Hong has applied for a patent on the new nanoparticles and is now testing them in animal models.
In tests against lab-grown strains of cancer, the nanoparticles boosted production of the immune stimulating protein interleukin-2 by T cells, one kind of immune cell in the body, by about 50 percent compared to no treatment. They were just as effective as antibodies. The nanoparticles were also able to improve the effectiveness of the chemotherapy drug doxorubicin in similar tests.
Normally, T cells produce a protein named PD-1 that acts like an off switch for immune responses. This “checkpoint” helps keep T cells from improperly attacking healthy cells.
Some cancer cells hide from the immune system by tricking checkpoints on T cells. They imitate healthy cells by producing proteins called PD-L1, which bind to the off switch and let tumors hide in plain sight. Several immunotherapies use antibodies — proteins that bind other proteins — against either PD-1 or PD-L1 to disrupt this connection.
“The key here is if you block that binding very efficiently, you can now reactivate the T cells, so the T cells start attacking the tumor cells,” says Hong.
But a course of those antibodies, known as checkpoint inhibitors, can cost upwards of $100,000 because pure antibodies are difficult and expensive to produce. Like these antibodies, the nanoparticles the researchers developed gum up the PD-L1 on cancer cells so they can’t activate the off switch on T cells. Hong’s lab used a different approach to achieve the same effect.
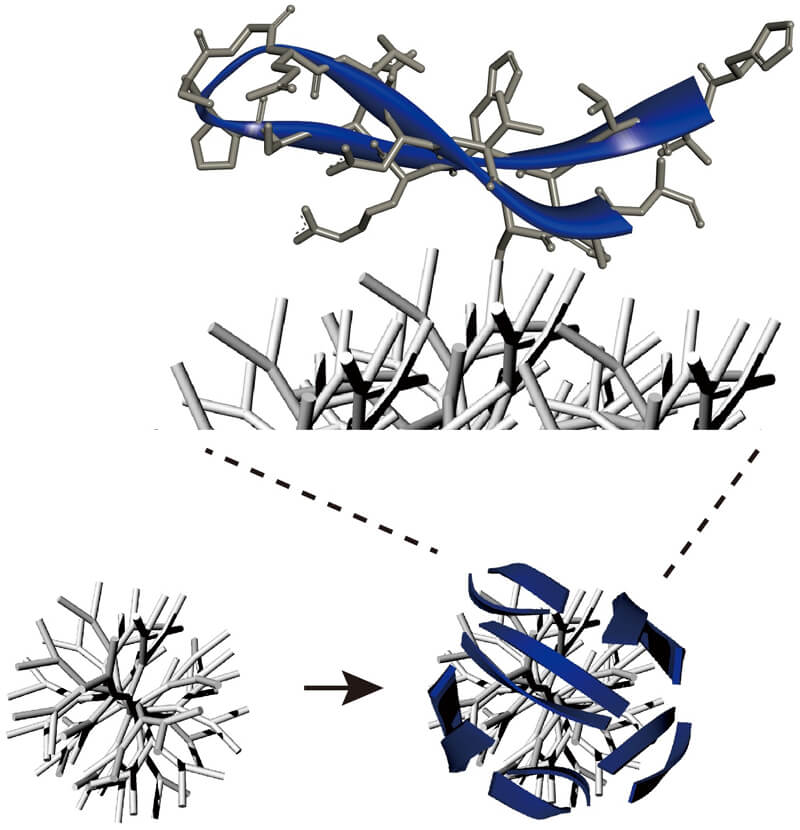
They took small chunks, or peptides, of the PD-1 protein and attached them to branched nanoparticles. The nanoparticles stabilize these peptides so they’re able to bind to PD-L1 on the cancer cells much like the full PD-1 protein can. They also have a lot of branches, so they can hold many copies of the PD-1 peptides and bind more strongly to PD-L1.
In test tubes, the nanoparticles attached to PD-L1 as strongly as full-sized antibodies did. A strong connection between the nanoparticles and PD-L1 means the cancer cells can no longer use these proteins to trick T cells.
Both the peptides and the nanoparticles they’re attached to are simple and cheap to produce in the lab. And both can easily be tinkered with and altered, so future research might be able to optimize them to work better by following this early proof-of-concept study.
“The bottom line is that, for the first time, we developed this peptide-nanoparticle platform for immunotherapy and found clear evidence that this system has great potential,” says Hong. “We’re looking forward to the next step.”
This work was partially supported by the National Science Foundation (grant DMR-1808251) and the National Institutes of Health (grants 1R01AR069541 and 1R21EB022374.)