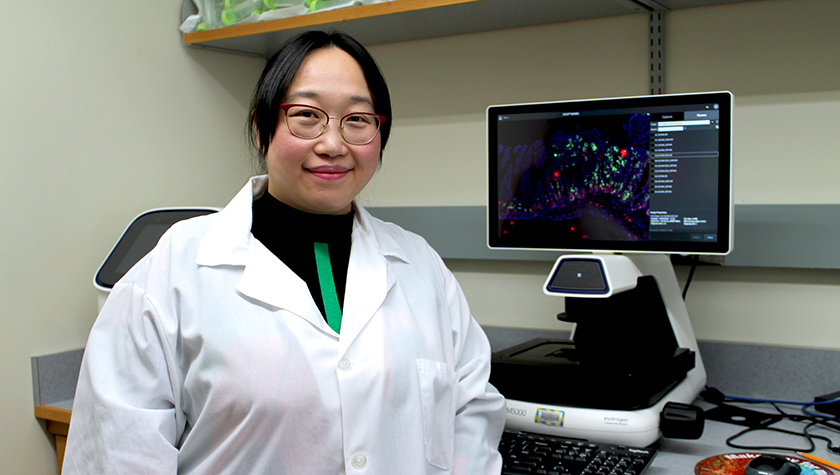
School of Pharmacy Assistant Professor Ting Fu and colleagues have identified a promising potential therapeutic lead for colorectal cancer
By Nicole Sweeney Etter
Scientists are still exploring all the possibilities of the trillions of microbes that reside in our gut, with implications from mental health to immune response. Now, new research at the University of Wisconsin–Madison School of Pharmacy shows that microbial bile acids could be a powerful new tool to fight colorectal cancer. Ting Fu, assistant professor of pharmaceutical sciences, and her colleagues recently discovered that a specific microbial bile acid, 3-oxo-lithocholic acid (3-oxo-LCA), can inhibit tumor growth in colorectal cancer.
It’s an area ripe for new treatments: Colorectal cancer is the second most common cause of cancer-related deaths, according to the American Cancer Society, causing a projected 53,000 deaths in 2025.
“I think this is a really promising therapeutic candidate for colorectal cancer,” Fu says. “Hopefully, our research can lay the groundwork for 3-oxo-LCA to be at least a drug lead.”
Testing the pathway
Microbial bile acids — which are produced when bacteria modify the host’s own bile acids — act as critical signaling molecules. Previous research has already shown that some microbial bile acids, including 3-oxo-LCA, have immune-modulating and anti-infection effects. These beneficial bile acids have also been found in higher levels in centenarians, suggesting they could have an anti-aging effect as well.
Now, the Fu Lab has discovered that 3-oxo-LCA has a novel anti-tumor function directly impacting epithelial cells, which line the inside of organs and are where most colorectal cancers originate.

The study, led by Fu and pharmaceutical sciences graduate student Fei Sun, was published this year in Cancer Research, in collaboration with the School of Pharmacy’s Professor of Pharmaceutical Sciences Jiaoyang Jiang, UW Department of Medicine Professor Dustin Deming, and collaborators from Arizona State University and University of British Columbia.
Fu’s group used multiple models to study disease mechanisms and test 3-oxo-LCA as a potential therapeutic. The anti-tumor effect was validated across three clinically relevant animal models (including an immune-deficient model), as well as in patient-derived organoid models. The Deming Laboratory in the McArdle Laboratory for Cancer Research provided the patient-derived colorectal tumor organoid, and the Jiang Research Group used computational modeling approaches to validate the biological findings.
Jiang calls the work of the Fu Lab “elegant.”
“I think these findings are exciting because they represent a new mechanism for gut microbiota and metabolites to impact human health and may offer a new opportunity for cancer treatment,” Jiang says.
The team identified a new mechanism of action for 3-oxo-LCA, finding that it induced rapid apoptosis, or programmed cell death, in cancer cells in both early and more advanced disease states. In addition to reducing existing tumor burdens, 3-oxo-LCA also limited the emergence of new tumors, highlighting potential roles in preventing tumor initiation as well as slowing progression.
“Some therapies slow cancer growth mainly by reducing inflammation or cell proliferation, which tends to be more effective in the early stages of tumor development,” she explains. “What makes 3-oxo-LCA especially promising is its ability to induce apoptosis. Because it directly triggers tumor cell death, it may remain effective even in more advanced tumors.”
When the researchers used pharmacological drugs to inhibit apoptosis, 3-oxo-LCA’s anti-tumor effect was significantly reduced, suggesting that it was the cell death that made it effective. Researchers also found that a specific nuclear receptor called farnesoid X receptor (FXR) — already elucidated by Fu as a target for treating inflammatory bowel disease and related cancers — plays a key role in inducing apoptosis. When Fu’s team knocked down the FXR in cancer cells, the anti-tumor effect of 3-oxo-LCA disappeared.
“What makes 3-oxo-LCA especially promising is its ability to induce apoptosis. Because it directly triggers tumor cell death, it may remain effective even in more advanced tumors.”
–Ting Fu
This work builds on Fu’s previous research on the role of the gut microbiome and its metabolites in colon cancer risk. But while other microbial bile acids she has studied can activate FXR and inhibit cell proliferation, 3-oxo-LCA is the first she has found that induces cell death.
“The new mechanism behind this one is why it is so dramatic in effect,” she says.
The patient-derived cancer organoid (PDCO) models and patient-derived xenograft (PDX) models, which used tumor tissue from human patients, provide strong evidence that 3-oxo-LCA might be relevant as a future therapeutic for humans. In addition, in vitro experiments demonstrated that 3-oxo-LCA induced cancer cell death in less than 10 hours — an encouraging sign of its efficacy.
While these models focused on colorectal cancer, it’s possible that 3-oxo-LCA could be effective in treating other cancers of the intestinal tract, Fu says.
Toward future treatments
Although funding is always a limiting factor, there is much more to explore, she notes. One future research direction could be to develop 3-oxo-LCA as a therapeutic drug. Further research could also illuminate what types of microbiomes naturally support the production of 3-oxo-LCA. Fecal microbiota transplant (FMT), which is already an approved treatment for other conditions, could help plant “healthy bugs” that generate 3-oxo-LCA, Fu says.
“That could be another route to treat the disease,” she says.
More analysis of the microbiome could also lead to precise nutrition options that support the production of 3-oxo-LCA.
“If we know the links and if we can have a formulation suitable for different types of people, maybe we can move intervention earlier so we can use this bile acid as a preventative dietary supplement rather than a drug,” she says.
This work is funded by Badger Challenge award (AAM7958), University of Wisconsin–Madison startup grants (AAI3795 and AAI3894), University of Wisconsin Carbone Cancer Center startup support (AAI5122), University of Wisconsin fall competition support from Wisconsin Alumni Research Foundation (AAL8735), PhRMA Foundation Faculty Starter Grant (2024-FSGDS-1161699), American Cancer Society Coaches vs. Cancer Bo Ryan-Jay Holliday Families Fund Research Scholar Grant (RSG-23-1150338-01), Margaret Q. Landenberger Research Foundation (AAM7699), and NIH R37CA288447 to T. Fu.
