Alum Apoorva Reddy (MS ’20, PhD ’23) leads new research revealing how CBD and THC differently influence sleep quality for people with cancer
By Susan Smith
Whether it’s due to pain, nausea, fever, or even chemotherapy itself, people with cancer often struggle to sleep. But sleep is exactly what their healing bodies need, improving quality of life, boosting the immune system while lowering inflammation and stress levels.
To get the rest they need, many turn to cannabis products to get a good night’s rest. But widespread cannabis use is racing ahead of research on how cannabis can help or harm sleep quality.
University of Wisconsin–Madison School of Pharmacy alum Apoorva Reddy (MS ’20, PhD ‘23) is working to fill this knowledge gap. As a postdoctoral fellow in the UW Department of Surgery, a position funded by the National Cancer Institute (NCI), she is running a series of studies in collaboration with surgical oncologists at the UW Carbone Cancer Center, exploring the influence of cannabis on sleep for people with cancer.
“Sleep is such a major issue for cancer survivors,” Reddy says. “More than half of cancer survivors report sleep disturbances, and they tend to be persistent. Even after 10 years of survivorship, some patients still report difficulty with sleep.”
Cannabis for sleep
To find answers, Reddy and colleagues analyzed data from 1,962 cancer patients enrolled in the Minnesota Medical Cannabis Program from 2015 until 2023, when recreational cannabis became legal in Minnesota. Patients obtained their medical cannabis from licensed dispensary pharmacists, and each time they picked up medical cannabis at the dispensary, they filled out a self-evaluation on symptoms.
“Although cancer patients were given medical cannabis for pain, nausea, or cachexia, many found it to improve their sleep,” she says.
The results of her analysis were a bit surprising.
Reddy and collaborators found that higher doses of cannabidiol (CBD), the non-intoxicating substance found in cannabis, resulted in clinically meaningful improvements in sleep quality in cancer patients. On the other hand, tetrahydrocannabinol (THC), known for its psychoactive effects, did not improve sleep significantly. Reddy says THC interferes with sleep quality, especially during the dream phase of sleep, also known as rapid eye movement, or REM, sleep. Since REM sleep is associated with emotional regulation and memory, long-term use of THC could impair mood and cognitive performance.
“After 30 days of use, CBD was associated with greater improvement in sleep than THC, and that was a surprise,” Reddy says. “THC can help you fall asleep faster with short-term use, but in the long run, it disrupts REM sleep. It is similar to alcohol in that regard. By disrupting REM sleep, THC can negatively affect memory and mood.”
At the beginning of the study, patients had an average sleep disturbance score of 6.72 out of 10, with 10 being the worst sleep quality. Analysis showed that patients taking CBD at the highest doses, more than 14.3 mg per day, showed an improvement of 1.87 points on the 10-point scale, while lower doses were associated with an improvement of 1.5 points.
“The route of administration didn’t affect their sleep scores; the amount of CBD did,” Reddy says. “With each 5 milligram increase in daily CBD dose, the odds of achieving a 30% or greater improvement in sleep increased by 4%.”

The study — with collaborators from the UW School of Nursing, UW School of Medicine and Public Health, and the Minnesota Office of Cannabis Management — was published in October in the Journal of Clinical and Translational Oncology. In the same month, she also published a review on cannabis for psychological symptom management and analyses on the association between cannabis and mood in cancer patients.
“We know that cancer survivors are using cannabis products, such as Delta-8 THC and Delta-9 THC, which are currently legal in Wisconsin if they are derived from hemp,” she says. Hemp is legally defined as any Cannabis sativa L. plant with less than 0.3% THC by dry weight, whereas marijuana is defined as greater than 0.3% THC by dry weight.
“Even though Wisconsin has several stores selling cannabis products, many Wisconsin patients acquire products from neighboring states, like Minnesota and Michigan, which have more stringent quality-control regulations than we currently do in Wisconsin,” says Reddy.
Research roots
Reddy’s interest in psychoactive medicine and sleep research began while she was a graduate student at the School of Pharmacy.
“I began my PhD the same year that CBD became federally legal in the United States and psilocybin received FDA approval for treatment-resistant depression. Patients with cancer were among the first to participate in studies showing that cannabis and psilocybin can support symptom management,” Reddy says. “I was fascinated by how these substances challenge the current gold-standard approach to evaluating cancer medications: the blinded, randomized, placebo-controlled clinical trial.”

During her graduate studies, Reddy also won a national competition sponsored by the National Center for Health Statistics (NCHS) for a data visualization on opioids and suicide, highlighting ways that policymakers could impact opioid overdose and suicide rates across age groups. She continued honing her visualization skills with Ryan Vandrey from Johns Hopkins University and presented nationally on a network analysis to visualize how common cancer symptom clusters are affected by cannabis.
“I think this is a useful method to understand psychoactive medicines that can affect multiple symptoms at once,” she says.
To train in psilocybin and sleep research, Reddy is working with Professor of Psychiatry Charles Raison.
“His clever study designs, his tenacity and resilience in researching psilocybin in the face of stigma, and his charisma when conveying complex ideas in a way that resonates with audiences of diverse educational backgrounds — these are just a few of Dr. Raison’s inspiring qualities,” she says. “It has been exciting to work with him as his mentee, advancing clinical trials on psilocybin formulations that may produce long-lasting improvements in well-being.”
Professor of Pharmacy Betty Chewning, her primary PhD advisor, also remains an important mentor.

“She is incredible,” Reddy says. “I hope to emulate her mentorship style for my own amazing student collaborators: Youning Zhao, Simerjot Kaur, and Sophia Melnyk. In the classes I teach, I try to recreate the engaging learning environment that she created for me.”
Reddy won first place for her educational research talk at the 2024 UW Postdoctoral Symposium, and she is currently a guest lecturer in courses on the science of cannabis at the School of Pharmacy and at the College of Agriculture and Life Sciences.
“Dr. Paul Hutson, who runs the UW–Madison Transdisciplinary Center for Research in Psychoactive Substances, helped me design a lesson plan for our pharmacy students focused on cannabis and neuropathic pain,” Reddy says. “I am so grateful to be able to tap into his wealth of knowledge in this area.”
Next steps
Reddy remains committed to advancing research and educational initiatives on psychoactive medicine.
“My long-term goal is to lead an independent research program focused on using psychoactive medicine to improve the quality of life and symptom control among cancer survivors,” Reddy says.
This year, she surveyed 650 Carbone Cancer Center patients about their cannabis use and perceptions. Almost one-third of their respondents reported using cannabis for symptom management after being diagnosed with cancer.
“Our team — which includes my phenomenal fellowship mentors, Dr. Heather Neuman, Dr. Kris Kwekkeboom, and Dr. Betty Chewning, has been working with the UW Survey Center and the REACH Program on this project,” Reddy says. “I hope to provide a platform for patients who could not previously speak aloud about cannabis use in Wisconsin. I will keep an open mind when analyzing the reported benefits and harms. My eventual goal is to find what product formulation helps while minimizing the chance of adverse effects.”
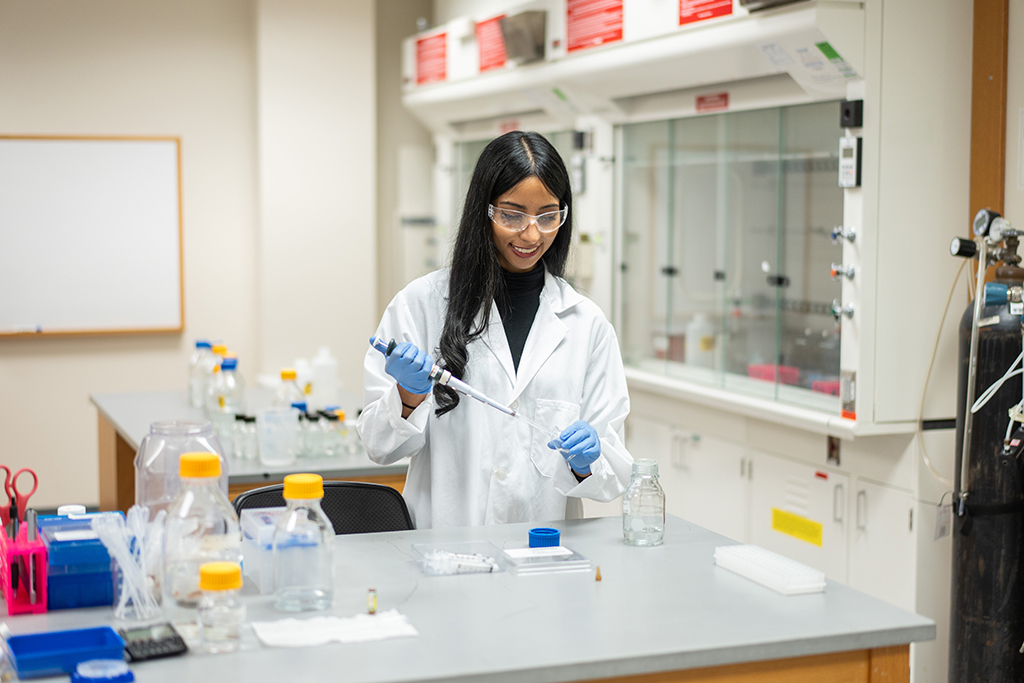
She is working with Professor of Pharmacy Barry Gidal, PharmD student Eden Lev, and the Zeeh Pharmaceutical Experiment Station to test how long cannabis products remain potent. They’re using high-performance liquid chromatography to analyze Epidiolex, currently the only FDA-approved CBD product, to determine whether it remains stable after the listed shelf life for an open bottle. Using Epidiolex as a proxy for the stability of other CBD products, the study could expand knowledge on how long these drugs will remain viable.
Reddy is also launching a study of employees at cannabis-dispensing locations in Wisconsin to see which THC and CBD products they think could be helpful for symptom management based on their experience and customer feedback.
In her free time, Reddy volunteers at Gilda’s Club, which offers support and education to cancer patients. From talking with patients, Reddy says, “there is so much curiosity” about cannabis products and whether they can be helpful or harmful as people are being treated for cancer.
“There are no formal, evidence-based guidelines on the hundreds of over-the-counter cannabis products that now exist. We’re hoping to contribute to the scientific body of knowledge to change that.”
–Apoorva Reddy
Reddy hears the same questions from health care providers, who currently do not receive standardized training on the use of cannabis products. This lack of knowledge could become more crucial if a pending bill to legalize medical cannabis passes the Wisconsin Legislature, which would position pharmacists in dispensaries to advise patients on cannabis use.
“I think all healthcare providers are looking for more guidance on cannabis; there are only guidelines for the use of the prescribed FDA-approved cannabis products. There are no formal, evidence-based guidelines on the hundreds of over-the-counter cannabis products that now exist,” Reddy says. “We’re hoping to contribute to the scientific body of knowledge to change that.”