The School of Pharmacy’s Community-Based Pharmacy Residency Program celebrates two decades of shaping residents, preceptors, and patient care
By Katie Ginder-Vogel
“Our goal was simple: to train pharmacists who could be true leaders in community practice — providers, advocates, and innovators in the spaces where care is most personal and often most needed,” says Mara Kieser, professor and assistant dean of experiential education at the University of Wisconsin–Madison School of Pharmacy.
That’s the founding vision behind the School of Pharmacy’s PGY1 Community-Based Pharmacy Residency Program, now celebrating its 20th year. Since it accepted its first resident in 2005, the program has graduated 64 residents across 17 sites. Residents have sought out the program from 24 states — as far as Hawaii — and hailed from 30 pharmacy schools.
“Reflecting back on this program’s 20 years, we celebrate the years that have passed, as well as the stories, relationships, and ripple effects of a program that has shaped — and continues to shape — community pharmacy in a meaningful way.”
–Mara Kieser
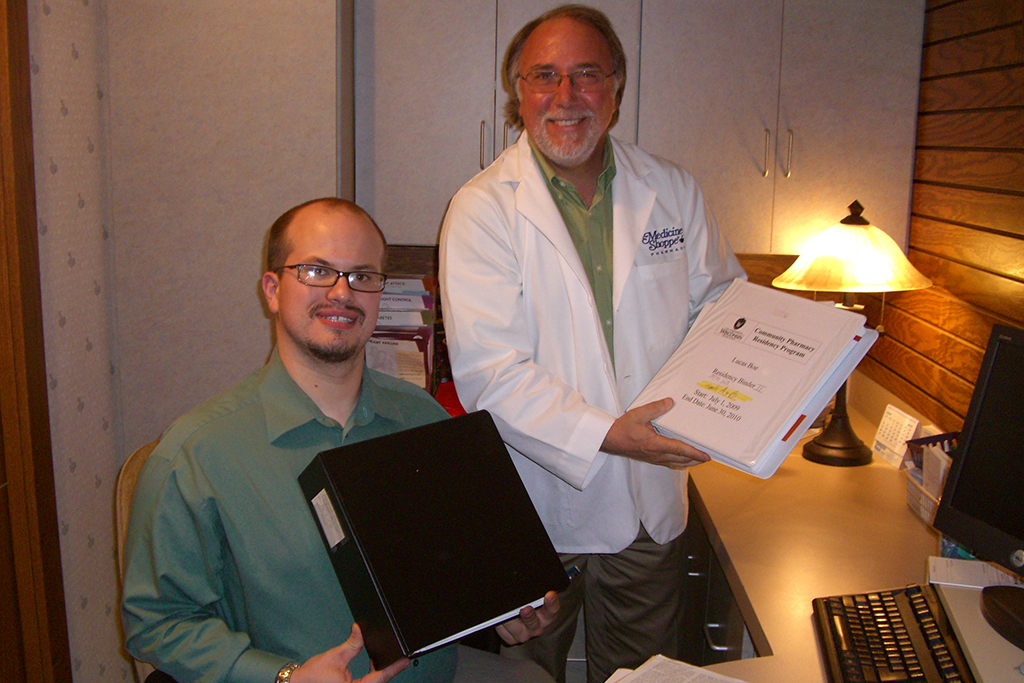
And it all started with a collaboration between Wisconsin pharmacists with a vision for leading patient care right from community pharmacies: Brian Jensen (BS ’80), at The Medicine Shoppe in Two Rivers, and John and Susan Sutter (BS ’78), at Marshland Pharmacy in Horicon.
“Reflecting back on this program’s 20 years, we celebrate the years that have passed, as well as the stories, relationships, and ripple effects of a program that has shaped — and continues to shape — community pharmacy in a meaningful way,” says Kieser, residency program director.
Roots of a vision
In the late 1990s, Jensen and the Sutters connected at an event, and the conversation gravitated toward residencies.
“John and Sue Sutter were with me. We talked about how we could get the whole idea of community practice residency aligned in our state,” Jensen says. “So I began to think about how we could do the first residency on our own, and I created my own goals.”

Curtis Johnson, a faculty member at the School of Pharmacy and friend of the Sutters, encouraged them to get involved.
“This is very much a story of mentors,” says Susan Sutter. “Chris Decker and Curt were interested in nurturing future practitioners and supporting innovative pharmacy practice, encouraging us. Brian, John, and I said, ‘Yeah, let’s give this a shot.’”
Decker, then executive vice president and CEO of the Pharmacy Society of Wisconsin, was a huge supporter of the residency program, and PSW was a supportive partner in accreditation at first. Marshland Pharmacy and The Medicine Shoppe became the first community practice residency sites in the state.
“We were the first site, and the Sutters came on board the next year,” says Jensen. “My first resident was Eric Geurkink (PharmD ’99), who is now at the Minneapolis VA. He had the courage to jump into the fray with me.”
“We used PSW as the founding and supporting umbrella, and we were accredited in 2002,” says Jensen. “The following year, we had meetings with the School of Pharmacy, because the program was aligned with what the School wanted to do.”
Jeanette Roberts, then School of Pharmacy dean, connected with Jensen and the Sutters to bring the community pharmacy residency program under the School’s purview.
“They had the vision to see the positive impact of this collaboration,” says Kieser.
Paired with the foundations already laid at Marshland Pharmacy and The Medicine Shoppe, the School of Pharmacy launched the PGY1 Community-Based Pharmacy Residency Program in 2005.
“Since community pharmacists are the most accessible healthcare providers, the School wanted to offer specialized training to elevate community pharmacy practice, like other pharmacy residencies,” says Roberts. “It beautifully aligned with the School’s mission to educate practitioners to practice at the top of their licenses and provide needed clinical services right there in the community.”
The program has grown to include 33 preceptors over its 20 years.
“It’s matured into a program that students interested in a career in community practice can complete to distinguish themselves,” says Sutter. “Having a year to implement some of the innovative patient care solutions that come out of community practice is viewed as well worth the investment.”
Improving care
Each resident takes the lead on a project designed to enhance patient care, streamline pharmacy operations, or otherwise strengthen the practice. Many of these projects, Sutter notes, continue to leave a lasting impact.
One of Marshland Pharmacy’s first residents, Beth Carlberg, undertook a project to smooth the process of filling numerous prescriptions sent home with patients after discharge from the hospital.

“Prescriptions were all still on paper at the time,” Sutter says. “Patients would be discharged from the hospital with a fistful of scripts to bring to the pharmacy, and we wanted to make the process of filling those more efficient for them.”
The resident helped the Sutters pilot a new process, in which hospital discharge patients all did an initial medication review with a pharmacist. The result was fewer billing errors and the ability to catch any duplicate prescriptions. Even after physicians started faxing or sending prescriptions digitally, the Sutters continued the practice until they retired in 2017.
“When patients come home from the hospital, they are so in tune to what their pharmacist has to say at that time,” Sutter says. “It’s a great, satisfying opportunity for pharmacists to talk with people then, and workflow efficiency frees up time for that great counseling experience.”
Sutter believes the community pharmacy residency program has positively impacted rural health.
“I’m a big advocate for rural health and the School’s commitment to it, and the Community Pharmacy Residency program started in more rural pharmacies,” Sutter says.
“We’re developing professionals who can navigate real-world healthcare challenges: medication access, health literacy, chronic disease management, and above all, relationships with patients and communities,” says Kieser.
Transforming careers
The residency program is just as transformational for residents as it is for patients and pharmacies.
“My residency changed my life and the trajectory of my career,” says Zachary Hovis, who completed his residency through the School of Pharmacy in 2014. He joined SSM Health, formerly Dean, to work on a pilot project for the health plan.

“The foundation of my residency was helping to start a pilot hypertension program,” says Hovis, now an assistant professor at the Medical College of Wisconsin. “I worked with Dr. Phil Bain at Dean East Clinic to develop a better way to track all of our patients with hypertension and help them stay in better control of their disease.”
Working from a list of patients who weren’t meeting their benchmarks for hypertension management, Hovis called them and talked with them about their medications, helping them decide whether to increase their medication doses or try a new medication. The project was so successful that Dean Health Plan hired him to help with medication therapy management. When SSM Health acquired Dean, they expanded the care model into new areas of chronic disease and promoted Hovis to primary care pharmacy supervisor.
Today, Hovis continues to use that experience as he oversees the hypertension clinic at Froedtert Hospital, using collaborative practice agreements to adjust patients’ pharmacotherapy.
“The residency was the perfect setting for me to absorb more information about how medications get from warehouses to patients’ hands,” says Hovis. “Talking with patients and seeing the processes is important for understanding how to help patients.”
Rachel Whitesitt had a similarly influential experience. She completed her PGY1 Community Pharmacy Residency at Streu’s Pharmacy Bay Natural in Green Bay, Wisconsin, where she is now clinical services manager. Her residency project involved implementing the Center for Disease Control’s National Diabetes Prevention Program at the pharmacy, and she has continued to apply for grant funding to improve the program.

At Streu’s, Whitesitt is involved in the Community Pharmacy Enhanced Services Network (CPESN) and was honored by PSW as the Wisconsin Distinguished Young Pharmacist of the Year in 2024. In addition to running Streu’s National Diabetes Prevention Program, she also handles antipsychotic injections, medication therapy management, and comprehensive medication reviews. She’s also come full circle, now serving as a preceptor in the program.
“I love precepting and seeing the growth and transition from student to pharmacist as students gain confidence and independence and begin to take initiative,” Whitesitt says. “The residency program is great. Being connected to a strong university like UW–Madison is a major asset to the program.”
Where the program is now
Although he’s now retired, Jensen is delighted by how far the program has come and what the former residents have achieved.
“The program is expanding, growing, and doing well,” Jensen says. “We want to prepare pharmacists to lead healthcare in their communities and world, and that’s what this does. It took a team to get this going, and the School continues to provide the structure and support to keep growing it. I’m so excited that the infrastructure that’s being put into place will sustain this model.”
“This residency has always been more than a steppingstone — it’s a launchpad for leaders.”
–Mara Kieser
Roberts agrees.
“It’s a challenge to coordinate all these moving parts, but a good one, and one our faculty have totally met,” she says. “Elevating the practice of community pharmacy, a cornerstone of healthcare accessibility — it doesn’t get much more important than that.”
Kieser, too, sees a field of opportunity, as provider status opens new realms of possibility for resident impact.
“This residency has always been more than a steppingstone — it’s a launchpad for leaders,” says Kieser. “And I have no doubt the best is still ahead.”