From artificial intelligence to better serving low-income patients, four UW alumni share how they’re improving pharmacy and healthcare
By Archer Parquette
Healthcare is constantly changing — and for the past few years, pharmacy changes have been in overdrive. There are new therapeutics, new processes, new standards and struggles, not to mention new technology like artificial intelligence that is reshaping the way the industry operates.
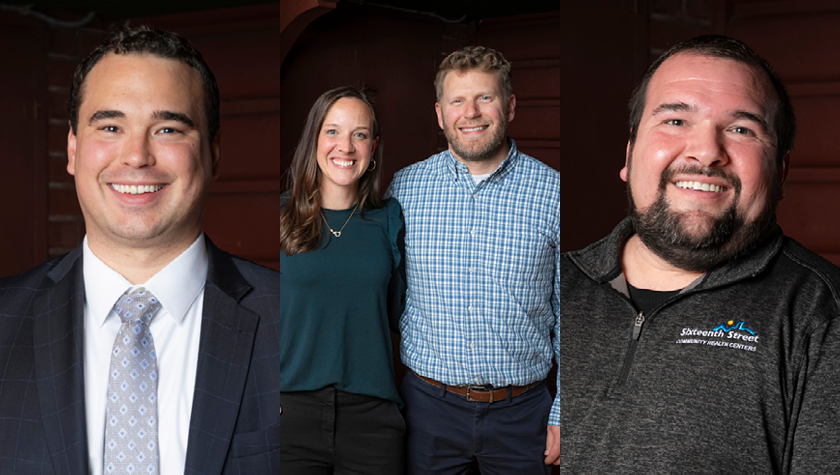
The University of Wisconsin-Madison School of Pharmacy and its alumni are on the front lines of the ever-evolving field — and pushing innovative new ways to take on healthcare challenges. Four Milwaukee-area School of Pharmacy alumni — Dean Bowen (BS ’16, PharmD ’20), Jessica (PharmD ’06) and Jesse (PharmD ’06) Schaetzel, and Jason Jenders (PharmD ’10) — shared their efforts, from developing new tech to better serving vulnerable populations, at a Milwaukee Innovators event on April 23.
“I find it incredibly inspiring to learn the innovative things our alumni are doing,” says Associate Dean for Advancement Dave Mott (BS ‘88, MS ‘92, PhD ’95). “Each is dealing with the challenges and complexities of our healthcare system, and they’re a huge source of pride for me as a graduate of the School of Pharmacy.”
AI in industry
Bowen is a field medical associate director at Sanofi, a global pharmaceutical company. In his medical role, Bowen is working on multiple clinical trials, including ones that are targeting disability progression for multiple sclerosis. He says the biggest change in practice is obvious — and it’s only just beginning.
“What I believe is going to completely transform the way we all practice in the next decade is the rise in the integration of artificial intelligence,” Bowen says. “AI isn’t just a buzzword anymore — it’s here. The highest levels of leadership across the healthcare industry are actively embracing it. It’s already started to impact how I work every single day. … AI’s power is truly astonishing.”

Bowen cautions that AI must be used with careful human expertise and guidance, but points out that it’s already making pharmaceutical work significantly more efficient. AI and large language models can analyze medical insights from hundreds of research reports and papers in only seconds, summarizing trends and even generating strategic plans based on that analysis.
“What used to take hours of manual review now happens in moments, freeing us up to spend more time acting on those insights,” Bowen says.
Bowen is also using AI to predict screening and enrollment rates for clinical trial locations and flag underperforming sites early, which allows the team to adjust the trials before underperforming sites jeopardize the timeline.
Those are just two of hundreds of current and potential AI uses.
“AI is poised to touch nearly every aspect of the profession, whether you’re in clinical practice, academia, or research. And it’s going to challenge us in the best way possible to rethink how we deliver value,” Bowen says. “I understand the concerns with automation, especially in pharmacy. But here’s what I truly believe — those who learn to work with AI, not against it, will be the future leaders of our profession.”
Harnessing data
The Schaetzels are also pushing technological innovation in pharmacy forward. The couple founded PharmASSIST Healthcare Dashboards two years ago, with the goal of offering healthcare teams efficient, easy-to-use access to the plethora of (often scattered) healthcare data.
In 2020, Jesse, who is the director of pharmacy for population health at Advocate Aurora Health in Milwaukee, began creating digital dashboards to make his work easier. The virtual tool took raw data and turned it into an easy-to-understand visualization that notes trends and key numbers.

“I was demoing one for somebody higher up in the organization, and afterward he said, ‘This is great, but how much does it cost?’” Jesse says.
He realized that the tool he had developed had higher potential than just a way to make his job easier. He expanded his dashboard efforts, making interactive tools useful for different healthcare applications, from analyzing long-term care facility patients to opioid stewardship. When the couple launched the startup, Jessica, who also co-owns Cedar Creek Apothecary in Cedarburg and was a long-term care pharmacist, spearheaded the business side.
“We focus our efforts on providing a customized service, tailoring whatever we do to meet the needs of the customer,” Jesse says.
Most recently, the state of Utah has tasked PharmASSIST with creating a dashboard to help with statewide opioid stewardship efforts.
“We work with a number of health systems and pharmacies throughout the country,” Jessica says. “Our motivations are to help make healthcare easier, more efficient, help with cost savings, and to really put value back where it belongs. If we can save time for healthcare workers on the front line then that is going right back into patient care.”
Community care
Jenders uses innovative practices and technology to better serve low-income and at-risk patients. Jenders’ pharmacy career took a turn when he met School of Pharmacy alum Nicholas Olson (PharmD ’03).
Jenders, a School of Pharmacy student at the time, completed a clinical rotation at the company where Olson was clinical manager, BioScrip. During this rotation, Jenders took care of patients battling cancer, HIV, and other diseases requiring specialty medications, which spurred a deep interest for him. After his graduation, Olson shared that he and Rick Fons (BS, ‘94) were opening a pharmacy for the AIDS Resource Center of Wisconsin — and Jenders immediately took them up on an offer to join the team.
“We had medical, behavioral health, dental, case management, pharmacy, and even a food pantry all in one building,” Jenders says. “Pharmacy was uniquely positioned to help our patients navigate all those services.”

At the same time, Jenders found that many patients living with HIV sometimes struggled to navigate the plethora of services or perhaps had broken trust for the healthcare system.
“The medication used to treat HIV had come a long way. The trick was really helping our patients with other aspects of their lives that they were struggling with, whether it is mental health, substance abuse, food security, or housing,” Jenders says.
Jenders helped spearhead a solution. The pharmacy staff identified which pharmacist or technician had the closest relationships with each patient who was struggling to achieve an undetectable HIV viral load, and then assigned those technicians or pharmacists to spend the next year following and supporting them on a routine basis. The staff also received training from other departments within the organization on how to best refer patients to their service line. Over 60% of the patients who received that personalized support reached a point where their viral load was undetectable for the first time since their HIV diagnosis.
Jenders has since taken over as the director of pharmacy at Sixteenth Street Community Health Centers (SSCHC) in Milwaukee, which provides medical services for underserved and uninsured patients. Like many health systems, workforce shortages have presented a challenge for Sixteenth Street, particularly for the Medical Assistant role. In response, he launched a clinical pharmacy technician program, which trains pharmacy technicians to support SSCHC medical assistants by handling refill requests, conducting patient outreach on medication access issues, and more.
“We have amazing, accomplished, innovative dedicated alumni. This makes me incredibly proud. We impact the lives of young people who go off and impact the lives of so many more in their careers as pharmacists.”
—Steve Swanson
“We’re really creating a unique role where technicians get to do something they’re excited about, and we’re filling the gap in the workforce,” Jenders says.
Recently, Jenders has also consulted with a company called Louvir to develop a tool that would allow federally qualified health centers (FQHCs) across the country to improve their 340B programs. The federal 340B program provides discounted prescriptions to community health centers and other eligible healthcare organizations like Sixteenth Street to help them serve low-income patients. The program involves large amounts of scattershot data, including wholesale records, data from outpatient pharmacies and more. Louvir compiled all the disparate data into reports that identified where FQHCs could better take advantage of their 340B resources. That data could then be used to track outcomes, such as medication adherence and refills, to target programs to better help patients.
“We have amazing, accomplished, innovative dedicated alumni. This makes me incredibly proud,” said Steve Swanson, dean of the UW–Madison School of Pharmacy, at the Milwaukee Innovators event. “We impact the lives of young people who go off and impact the lives of so many more in their careers as pharmacists.”


















