10
September

Across the world and close to home, these recent School of Pharmacy alums are making a difference
By Jessica Steinhoff
The fourth annual Five of the Future feature highlights the adventures and accomplishments of alumni from the University of Wisconsin–Madison School of Pharmacy’s five major degree programs: Bachelor of Science in Pharmacology and Toxicology (PharmTox), Doctor of Pharmacy (PharmD), Master of Science in Health System Pharmacy Administration, PhD in Health Services Research in Pharmacy (HSRP), and MS or PhD in Pharmaceutical Sciences (PharmSci). And these changemakers are just getting started — all of them have graduated within the last 15 years.
Our 2024 group includes the creator of a medical education smartphone app, a world traveler running a field hospital for Afghan refugees, a health outcomes expert helping rare-disease treatments reach patients, a health system administrator extending the boundaries of clinical pharmacy practice, and a researcher working on new ways to deliver biologic therapies.

Location: Milwaukee, Wisconsin
Position/Employer: Medical student, Medical College of Wisconsin
Claim to Fame: Co-founding ChatClinic, a medical education platform that helps students build clinical skills through simulated patient interactions
Proudest moment: Discovering that medical educators in other states — and across the globe — are following ChatClinic’s evolution
Inspiration: The thrill of learning something new
Nathaniel Verhagen (BS ’21) didn’t know what his major would be when he arrived at UW–Madison. He knew he had to join the Wisconsin Badgers Crew. Though he’d never rowed before, he sensed the opportunity would pay off if he seized it.
“I learned how far I could take not only my body but my mind,” Verhagen recalls.
This knowledge has served him well ever since. It propelled him through the UW–Madison School of Pharmacy’s Pharmacology and Toxicology program, into medical school at the Medical College of Wisconsin (MCW), and into the world of artificial intelligence and medical education tool development.

ChatClinic, a novel web-based application he co-founded, came from pondering the possibilities of large language models like those that power ChatGPT. It uses artificial intelligence to help medical students improve their clinical skills.
Clinical skill-building is like weightlifting, according to Verhagen: The more repetitions you do, the stronger you’re likely to become.
“ChatClinic is about giving students more repetitions of certain kinds of patient encounters, which can help them gain clinical skills more efficiently,” he says. “If a fourth-year medical student like me goes through as many repetitions as a resident physician has typically done, patients should receive better care.”
To turn this concept into a product, Verhagen leveraged one of his strengths: connecting super-talented people. His fellow co-founder is a basketball buddy and MCW classmate who used to work in software engineering. A professor with expertise in machine learning has provided additional expertise and support. He has even led a team of local high schoolers as a project manager for their digital communications class to produce media supporting ChatClinic’s mission.
“When other people see the benefit of what we’re doing with ChatClinic, it makes us go further.”
—Nathaniel Verhagen
ChatClinic’s technology utilizes a bank of expert-reviewed patient cases to craft AI-generated scenarios for the student user to navigate. First the student chooses a specialty to practice. Then they receive a simulated patient’s demographic information and reason for seeking care. A conversation with the patient unfolds through messaging using a chatbox. The student can even order tests, and the results correspond to a diagnosable condition.
“This process helps medical students learn which questions are the most important to ask in different situations,” Verhagen says.

ChatClinic can also benefit students in other health care disciplines. MCW pharmacy students became some of its first users following its public debut in May 2024. After studying kidney injuries in class, they used ChatClinic to engage with the content in a different way.
“We surveyed them afterward, and almost everyone indicated they want more technology like this,” Verhagen says.
The app is being integrated into MCW’s medical education curriculum, and Verhagen says it’s on the radar of several other schools. Though becoming an otolaryngologist — an ear, nose, and throat surgeon — is his main career goal, he hopes ChatClinic’s journey is just beginning.
“When other people see the benefit of what we’re doing with ChatClinic, it makes us go further,” he says.
Back to top
Location: Doha, Qatar
Employer/Position: Director of pharmacy, International SOS
Claim to Fame: Running the United States’ largest COVID-19 mass-vaccination site
Proudest Moment: “When I found out about my current job at an Afghan refugee camp in Qatar, I reached out to the pharmacists and techs I’d worked with at an Afghan refugee camp in New Jersey and asked if any of them might want to join me. Every single one, except for somebody who was in school, said yes. They were willing to drop whatever they were doing to come work with me again.”
Inspiration: “I want to understand what’s going on around me, and it’s important that I understand things for myself. That’s one reason I travel. I like to see how people live in other parts of the world instead of being told.”
“I like creating,” admits Greg Sitter (PharmD ’12). “Give me a blank slate and I’ll build a functional system from scratch.”
This talent for turning nothing into something special saved the day repeatedly at a COVID-19 vaccination site in Oakland, California. It was 2021, and Sitter had just returned from a year of backpacking following 14 years working at Wisconsin-based retail pharmacies, first as a technician and later as a managing pharmacist.

“I stumbled into running the nation’s largest mass-vaccination site by accident,” Sitter says. “I showed up to keep track of temperatures and keep vaccines stable and ended up in charge of most of the operation.”
A few months later, a federal employee who’d noticed Sitter’s resourcefulness asked if he’d help at a new camp for Afghan refugees on the East Coast. Eager for a new adventure, Sitter signed on. He had no idea chaos awaited him in New Jersey.
“When I arrived, the site was a collection of tents in a field. All I had were a chair and a lockbox. We had garbage bags filled with medication and no real system in place,” he remembers. “I created everything needed for the pharmacy operation, from formulary documentation processes to an inventory system.”
Sitter quickly learned about the challenges Afghan refugees face, including low literacy levels. After hiring someone to translate prescription labels into the languages most Afghans speak, he discovered that a majority of the population can’t read or write.
“I like creating. Give me a blank slate and I’ll build a functional system from scratch.”
—Greg Sitter
“This means lots of people can’t read traditional prescription labels,” he says. “In Afghanistan, they use a system of dashes and circles to show how many pills to take and how many times a day. It’s ingenious and it works, so we use it.”
In addition to helping more than 18,000 refugees get medical care, Sitter forged relationships with his 25-person team and International SOS, the company running the camp. International SOS provides medical clinics and security personnel to expatriates and global organizations. In August 2023, Sitter moved to Qatar to become its director of pharmacy operations and helm another refugee camp.

A few months before departing for Qatar, Sitter visited Antarctica, fulfilling his dream of setting foot on all seven continents.
“Traveling there felt like being teleported, and when we arrived, we saw so many penguins, as well as seals, dolphins, and whales, which came surprisingly close to the ship,” he says. “It was a great learning experience, and it was fascinating to see the limited human impact when we stepped off the ship.”
In Qatar, Sitter is constantly learning. He also applies what he learned through the New Jersey camp and his clinical training in the School of Pharmacy’s PharmD program. Though Sitter hopes to return to the States someday, and possibly work as a medical science liaison, he’s grateful for the opportunity to help people in need.
“These refugees come to us with nothing, and we’re their first sign of what Americans, other than soldiers, are like,” he says. “That’s as rewarding as it gets.”
Back to top

Location: Edwardsville, Ill.
Employer/Position: Associate Director, Takeda Pharmaceuticals
Claim to Fame: Studying respiratory health outcomes with the Illinois Department of Public Health to help identify health disparities.
Proudest Moment: When her PharmD student mentees find success in nontraditional pharmacy careers
Inspiration: “Improving patient health is my North Star. Everything else pales in comparison.”
Transitioning from academia to the private sector can be a bumpy road, but Maithili Deshpande (PhD ’13) makes it look easy. When facing obstacles, the graduate of the UW–Madison School of Pharmacy’s Health Services Research in Pharmacy (HSRP) program remembers that her work can improve real people’s quality of life.
After graduating from the UW–Madison School of Pharmacy, as a professor at the Southern Illinois University Deshpande was focused on health disparities research in respiratory health. She’s especially proud of her health outcomes research collaborations with the Illinois Department of Public Health and local health systems.

“I was part of a working group that identified asthma trends throughout the state of Illinois by performing a county-level analysis of asthma-related mortality, morbidity, and quality of life,” she says. “Counties could use this information to track the state of asthma and drive asthma specific education or intervention programs.”
Identifying health disparities and helping health systems better understand them were important parts of Deshpande’s research. She collaborated with a health system in one Illinois county to understand if there were geographic patterns associated with poor asthma outcomes. Assisted by a geographic information systems (GIS) collaborator, they found that patients from neighborhoods with older housing made more hospital emergency department visits for respiratory concerns.
“If physicians know that a patient lives in an older neighborhood with older homes, where issues with dust and allergens are more common, they can suggest a home assessment that looks for common triggers for asthma and chronic obstructive pulmonary disease,” Deshpande says.
In addition to the research, she enjoyed teaching PharmD students about population health and health outcomes research. She helped many find fulfilling alternative pharmacy careers — which inspired her own career transition.
“Knowing that there aren’t many treatment options for people with rare and debilitating diseases, that pushes me forward.”
—Maithili Deshpande
“Helping students explore industry pathways got me thinking about my career, and I realized that there is so much more to learn, which is why I transitioned to my current role in neuroscience at Takeda Pharmaceuticals,” she says. “Knowing that there aren’t many treatment options for people with rare and debilitating diseases, that pushes me forward.”
This is especially true in Takeda Pharmaceuticals’ neuroscience space, where Deshpande facilitates the evidence generation strategy. As an associate director, she leads a team that develops the evidence new products need to get approved and go to market.
“Making it through the regulatory and commercialization processes requires a robust plan for gathering and presenting evidence,” she says. “I have a deep appreciation for how long it takes to bring a drug to market because I know how many things have to fail first to eventually make it to that point.”

Deshpande must think like both a scientist and an architect, choosing the most compelling pieces of evidence for different situations and building a convincing case for bringing a drug to market. In addition to a successful clinical trial, drugmakers must also show that there is a significant unmet need, and that their product is necessary for treating the disease it targets, as well as cost-effective for payers.
The rare-disease treatments Deshpande works with face even taller hurdles. Drug development programs face significant complexities such as limited sample sizes for trial recruitment, lack of consensus on the outcome measures that are valuable to assess, as well as challenges in communicating evidence to regulators and convincing payers.
“In such cases we engage with patients, physicians, regulators, and payers early on in drug development to truly understand the evidence needs for the drug development program,” she says, “Ultimately, the goal of serving in rare disease is to advocate and facilitate the needs of an often-underrepresented community.”
Back to top

Location: Boston, Mass.
Employer/Position: Senior Scientist II, Elektrofi
Claim to Fame: Helping to make biologic therapies safer and easier to self-administer
Proudest Moment: “The moments at Elektrofi that have helped me grow. Our multidimensional approach to problem-solving has made me think not only about what will solve a problem, but which solutions are efficient, easy to implement, and likely to improve patients’ lives.”
Inspiration: “Elektrofi is located in a building with multiple biotech startups, so I meet people working on solving different problems in healthcare. I’m constantly amazed by the new ideas. It’s a great environment for innovation.”
Ashita Nair (PhD ’21) is a puzzle solver of the highest order. As a senior scientist at Elektrofi, a biopharmaceutical formulation tech startup, she gets to grapple with questions involving every part of the business.
“Each day we tackle questions together, everything from ‘Would the patient feel pain if this suspension is injected?’ to ‘Would the FDA find this acceptable?’” says the graduate of the School of Pharmacy’s Pharmaceutical Sciences program. “I love this aspect of startups: It’s exciting to get a holistic view of the drug development process.”

Nair joined Elektrofi when it had 30 employees, and it’s growing fast. The company’s proprietary drug-delivery system is fueling this expansion. Nair says it could revolutionize the way patients receive biologic treatments.
“Right now, if a doctor prescribes a biologic therapy, the patient gets an infusion at a hospital, which takes a few hours. Our technology converts that therapy into a subcutaneous dose the patient can administer at home,” she explains.
The treatment is delivered through an Epipen-like autoinjector and takes seconds rather than hours. Nair leverages her expertise in drug delivery systems, polymer-based nanoparticle design, cancer biology, and extracellular vesicles to make it safe and easy to deliver.
“My job is to find the best composition, one that enables the proteins to stay intact during this proprietary process and shelf stable over the long term,” she says.
“Working in drug development helps me apply my skills to any problem, professional or personal, in a flexible way.”
—Ashita Nair
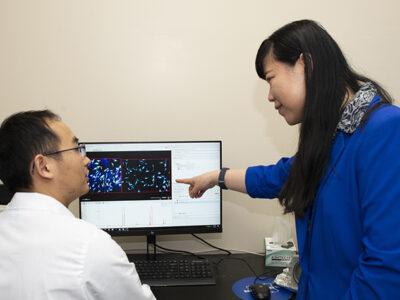
Nair’s work in the School’s Hong Research Group, led by Professor of Pharmaceutical Sciences Seungpyo Hong, was excellent preparation for her current role. She specialized in creating delivery systems for cancer-fighting gene therapies, advancing scientific knowledge about how to boost the selectivity of therapeutic agents while reducing toxic side effects. Combining desirable properties of natural exosomes and synthetic dendrimers was an essential component of this work.

“The dendritic system is modular enough that we can conjugate different targeting agents to the same polymer, and we could design [these agents] in a way that targets different parts of the body,” she says.
In addition to bringing this knowledge to Elektrofi, Nair’s leadership acumen helps teams of biologists, engineers, and clinicians collaborate effectively. Having worked in Singapore, Canada, the United Kingdom, and the United States, her cross-cultural communication skills are an asset as well.
“Working in drug development helps me apply my skills to any problem, professional or personal, in a flexible way,” she says.
Back to top

Location: Boston, Mass.
Employer/Position: Director of Pharmacy, Mass General Brigham Healthcare at Home
Claim to Fame: Using an engagement-building dashboard to transform employee culture at Massachusetts General Hospital
Proudest Moment: “I wasn’t even a year out of residency when the COVID-19 pandemic hit, but I saw it was a huge learning opportunity. I learned a lot about crisis management and how to lead people who are trying to take care of patients and themselves.”
Inspiration: “When I look back at my career, I want to know I made a difference in the profession that has made a difference in my life.”
“Empowered clinical pharmacists can truly make a difference in patients’ lives,” says Katherine DeSanctis (MS ’19).
DeSanctis knows because she used to be one — and still is at heart. In her clinical work, patient interactions were key moments to effect change, whether helping a patient improve their diet or explaining why their insulin might not be working. As she thought about her future, she realized she wanted to help other pharmacists thrive.

The combined master’s degree and pharmacy residency in Health System Pharmacy Administration at the School of Pharmacy and UW Health was an ideal place to prepare for a leadership role.
“I liked that I could take engineering and business courses that I could apply to hospital operations,” she says.
After graduating in 2019, DeSanctis stepped into a management position at Massachusetts General Hospital. Within three years, she became director of pharmacy operations, leading a large team in its central distribution, compounding, and perioperative pharmacies. This work earned DeSanctis national recognition from Becker’s Hospital Review in February 2024.
One accomplishment involved boosting employee engagement and retention during the COVID-19 pandemic. Posting operations announcements in a central location kept email deluges from overwhelming exhausted pharmacy workers. A dashboard was developed to deliver information about different initiatives at a glance. It also provided a way to share constructive feedback, prompting staff to identify specific problems and possible solutions.
“Showing employees we heard them and communicating the ‘why’ behind decisions helped make this successful,” DeSanctis says. “A culture change happened; we became more bidirectional and conversational.”
“Empowered clinical pharmacists can truly make a difference in patients’ lives.”
—Katherine DeSanctis
The conversational piece matters greatly to DeSanctis, who prioritized getting to know each Mass General pharmacy employee.
“I wanted them to see that I understood the work they were doing, and I tried to be transparent about what was coming down the pipeline,” she says.
Increasing pharmacist engagement is also a goal at Mass General Brigham Healthcare at Home, which provides acute care where patients live. DeSanctis became its director of pharmacy in November 2023. In this role, she shapes clinical pharmacy operations at five hospitals where beds are few and far between.

The program aims to improve patient outcomes by receiving care in the comfort of their own home, while at the same time freeing up hospital beds for those who need them most. DeSanctis hopes to make clinical pharmacists more available to its patients.
“I’d like to have a pharmacist who goes into homes and helps with transitions of care, when patients leave the hospital to manage their care at home, which can be hard for patients to navigate,” she says.
Pharmacists can also benefit medical providers delivering home-based care.
“Every time I shadow a nurse, questions for the pharmacist come up, which tells me that having a pharmacist there is valuable,” DeSanctis says. “I feel fortunate to be in a position where I can advance clinical practice in this way.”
Back to top