
13
March

Associate Professor Olufunmilola Abraham’s opioid safety video game reaches the point of prescription: emergency departments
By Katie Ginder-Vogel
It’s tough to be a teenager, as increasing responsibilities and social pressures meet a growing sense of independence. Add to the mix sports injuries and wisdom teeth removals, and for many, the teenage years also become a first exposure to opioids.
A 2021 study found that nearly 19 percent of adolescents had used opioids in the previous year — but only 15.7 percent were using them as medically prescribed.
To teach teens what they need to know, Olufunmilola Abraham (MS ’11, PhD ’13), associate professor in the University of Wisconsin–Madison School of Pharmacy’s Social and Administrative Sciences Division, began developing the first digital game to educate teens about medication safety in 2018: MedSMA℞T.
“It’s so important as a social scientist to think about what people enjoy in their daily lives,” says Abraham. “How can we study those things — games, for example — and leverage them as health interventions?”
After years of testing and honing the game, Abraham and collaborators recently concluded an 18-month pilot study of the groundbreaking game’s implementation in the UW Health Emergency Department, examining the feasibility and effectiveness of using a game to teach youth about opioid use and misuse.
An evolving intervention
Abraham began her journey with MedSMA℞T in 2018 when the UW Institute for Clinical and Translational Research (ICTR) funded her proposal to build the first iteration of the game using a community-engaged approach and a systems engineering lens. Her research group, the CRoME team (Collaborative Research on Medication Use and Family Health), uses novel approaches to improve medication safety and health behaviors for vulnerable patients, and multiple stakeholder groups provide regular feedback on her projects.
“We have a youth and student-focused lab, so we focused on the user from the beginning — how they’d want to learn about opioid use,” explains Abraham. “With Gear Learning at the UW, we designed a prototype that included stories and feedback from youth — how they receive opioids, what it looks like to have them in the home, how they interact with their peers.”
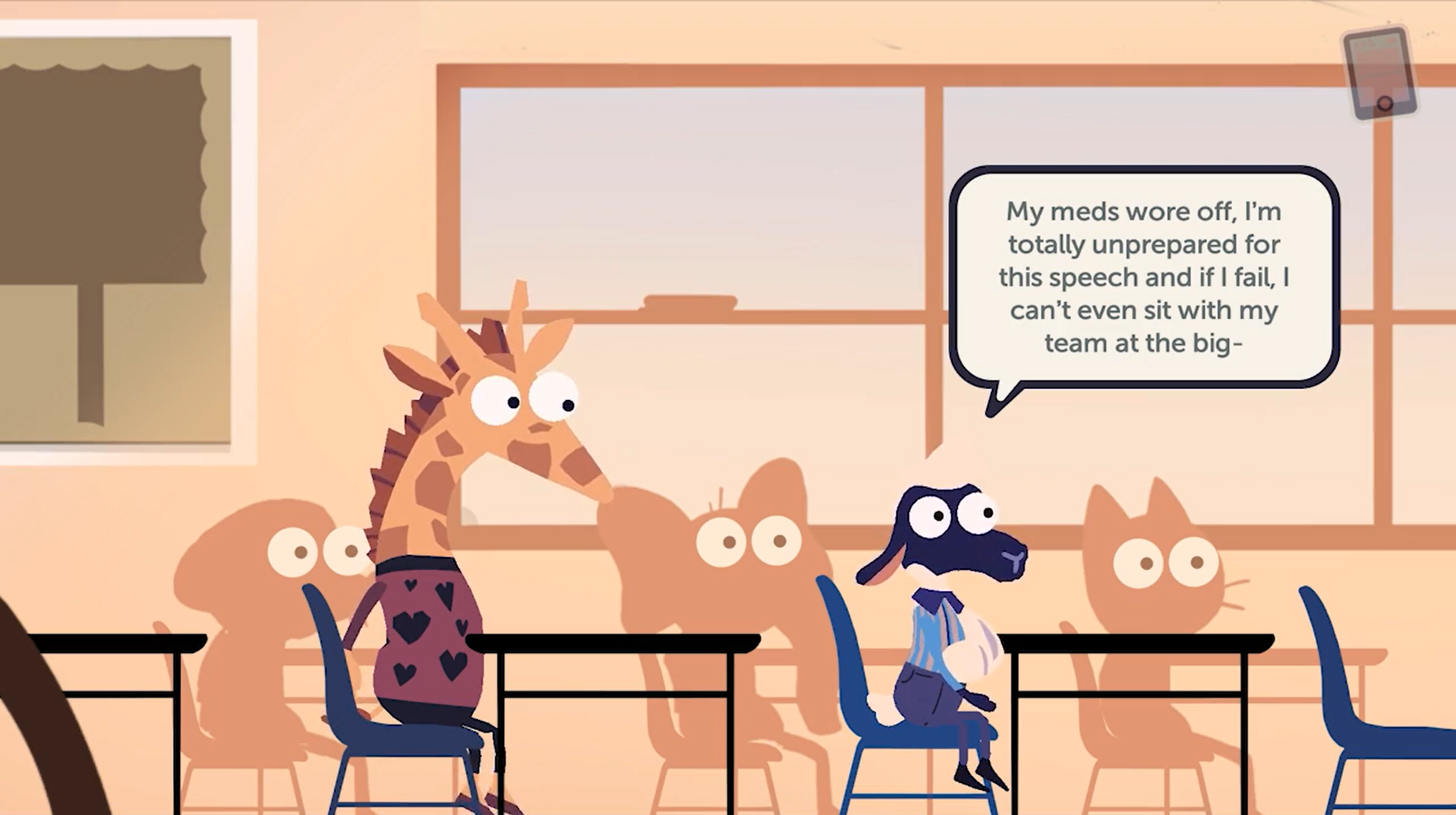
School of Pharmacy information processing consultant Eric Robinson programmed the second iteration of the MedSMA℞T game, which features anthropomorphized animals navigating scenarios relating to safe opioid use and storage. For example, one character receives prescription pain relievers for a broken arm, and then her friends come over. Her prescription is on the counter, and while she isn’t looking, her friends take some and get sick — how could this have been prevented with safe storage? Another character has some leftover medication from a sports injury, and his friends ask to buy some. If the player chooses to sell them, a friend could die of an overdose, giving a realistic sense of the risks involved.
Abraham’s team refined the game in partnership with local schools, thinking that’s where young people would prefer to learn about opioids. However, interviews with the teens revealed that they preferred to learn about safe medication use in a clinic and community settings, for example at points of prescribing and dispensing of these medications.
When Abraham’s research group heard from parents who wanted to play the game, they got a grant from the UW Prevention Research Center to test the effectiveness of kids and parents playing the game, followed by a discussion about medication management at home. The pairing of the game and discussion became MedSMA℞T Families.
“We had the opportunity to take up the challenge with community stakeholders, and MedSMA℞T Families is now a two-part intervention,” says Abraham. “The first part is the game, MedSMA℞T: Adventures in PharmaCity. The second part, after the parent and child play the game, is for them to talk about it and work together to develop a personalized family medication safety plan.”

MedSMA℞T Families has been piloted with more than 70 parents and teens and more than 20 pharmacists for potential deployment in various pharmacies across three health systems.
School of Pharmacy Associate Dean of Experiential Education Mara Kieser suggested that the School could use the game with fourth-year PharmD students doing community Advanced Pharmacy Practice Experience (APPE) rotations. Now, when participating pharmacies in Wisconsin distribute an opioid, pharmacists and APPE students are able to offer patients the opportunity to play the game as part of their medication counseling.
Abraham conducted a small pilot to gather pharmacists’ responses to the game, which resulted in an article in Pharmacy.
“Twenty-two pharmacists across Wisconsin said, ‘This is helpful; we would use this, and here are some suggestions to facilitate the use of MedSMA℞T Families in pharmacies,’” says Abraham.
Educating at the point of prescription
It was Abraham’s mentor — Manish Shah — who suggested using the game in an emergency department (ED), where opioids are prescribed. Abraham partnered with Irene Hurst, assistant professor in the UW Division of Pediatric Emergency Medicine. The two became co-investigators on an 18-month study of the game’s implementation in UW Health emergency departments, funded by the 2022 Dissemination and Implementation Research pilot award program, which is co-sponsored by ICTR and the Wisconsin Partnership Program (WPP).
The UW Health Emergency Department clinicians and recruitment team were enthusiastic about the project. For the course of the study, teen patients who were prescribed an opioid medication in the adult and pediatric emergency departments had the option to play the game, as did their parents.
“If we want uptake in clinical settings, pharmacists and clinicians need to be equal players in informing research, intervention design, and use.”
—Olufunmilola Abraham
“Parents are gatekeepers of medication in the home, so we’ve got to include them,” says Abraham. “If we want uptake in clinical settings, pharmacists and clinicians need to be equal players in informing research, intervention design, and use. I think that’s why we’ve been successful — our thoughtful, inclusive approach.”
The research team — including School of Pharmacy Health Services Research in Pharmacy graduate students Tyler McCarthy and Sarah Nadi, and the Department of Emergency Medicine’s Phoebe Natzke and Alden Laev — met monthly to ensure a fluid implementation.
“Our ED staff played the game and gave feedback and have expressed a lot of positivity about the trial,” says Hurst. “I work clinically in the ED, and seeing families play the game was positive for me, both in terms of being involved in the study team and seeing in real time how people were using it and using the information.”
Parents and teens were eager to participate in the opportunity to learn more about safely navigating opioids, says Laev, UW Health’s ED research coordinator.

“The ongoing interactions between the ED research coordinators and the patients participating in the study allowed us to provide real-time feedback to Dr. Abraham and her team about the educational game,” says Laev. “This collaboration leveraged diverse perspectives among patients and providers to refine the intervention, which we hope will further next steps in this important line of research.”
In addition to clinician and patient feedback, Abraham also has data from the game itself that she can use to further understand its usage.
“We developed in-game analytics to learn how people play the game and interact with it,” says Abraham. “When players complete a survey on their understanding of opioid safety, we will examine game data to see if what they do in the game translates to their real-life thinking.”
In the past year, Abraham has published seven articles about the game, including two in the Journal of the American Pharmacists Association, that detail pharmacist and adolescent reactions to the game, how it opens a dialogue between teens and parents, and how the game holds promise as a widespread intervention that could be adapted for other health topics for teens.
“The power of our partnership made the project successful and enjoyable,” says Abraham. “I’ve been using it as a model for how to collaborate in a really successful, meaningful way with other UW Health settings as we expand the games we’re working on.”
Continuing the mission
Now that the 18-month study is complete, Abraham, Hurst, and their colleagues are reflecting on what they’ve learned, celebrating successes, addressing opportunities, and preparing for the game’s next phase.
The team’s next step is to develop MedSMA℞T Mobile — the most common player suggestion was to create a mobile version of the game, which had been designed for Chromebooks in schools. They have applied for a grant to partner with Filament Games in Madison to create a mobile version of the game and update the game’s features and educational content. Abraham has already made partnerships to implement the mobile version in multiple emergency departments across Wisconsin, including UW Health.
“I’m excited for the next chapter of MedSMA℞T and to keep rolling it out locally in community hospitals and UW, as well as further outreach in Wisconsin,” says Hurst.





