9
March

Professor Seungpyo Hong continues to advance technology to track circulating tumor cells, which could lead to a more effective, easier way to monitor cancer progression
By Nicole Sweeney Etter
For decades, researchers have known that circulating tumor cells (CTCs) in a patient’s bloodstream could hold the key to accurately monitoring cancer progression — providing answers through a simple blood draw instead of painful biopsies or burdensome scans that don’t always catch wandering cancer cells. But to harness the full power of these hard-to-find CTCs, researchers had to overcome technical hurdles.
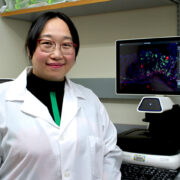
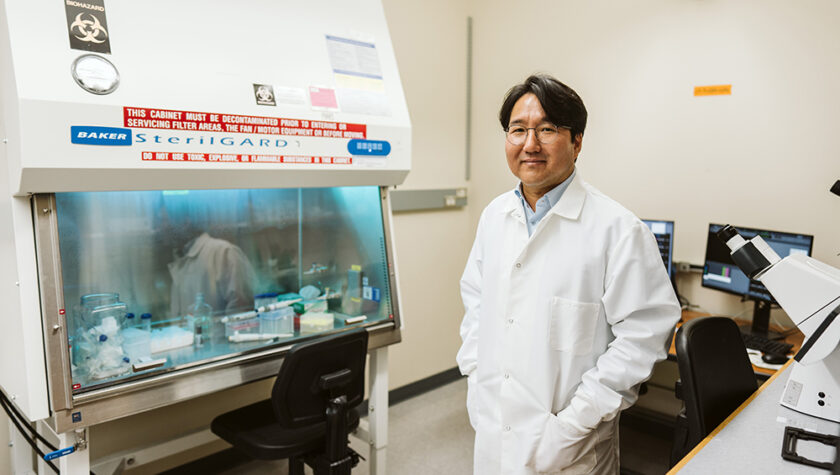
It’s a challenge that University of Wisconsin–Madison School of Pharmacy Professor Seungpyo Hong, of the Pharmaceutical Sciences Division, has been chipping away at since 2008.
“We came up with an idea to make detection and analysis of CTCs much better than other technologies,” says Hong, the Milton J. Henrichs Chair in Pharmaceutical Sciences and director of the Wisconsin Center for NanoBioSystems (WisCNano). “A simple blood draw is going to help get information about the disease and the current status of the patients, and it’s going to help the physicians come up with the best possible solution.”
“We are trying to ultimately translate this technology to the clinic so that we can directly help patients.”
—Seungpyo Hong
Now Hong is closer than ever to achieving his goal. He is partnering with clinicians across the United States and Korea to test his technology and publishing promising results across different cancers. Capio Biosciences, the startup he co-founded, is manufacturing the second-generation prototypes of the CTC capture technology — dubbed CapioCyte — first targeted for use as a research-use-only (RUO) device. That brings his research team one step closer to eventually getting the technology approved by the U.S. Food and Drug Administration (FDA) for widespread clinical use.
“We are trying to ultimately translate this technology to the clinic so that we can directly help patients,” Hong says.
Using nanotechnology to improve outcomes
There are good reasons to improve standard cancer monitoring methods. Not only could it make cancer monitoring more comfortable for patients, but it could also improve their treatment outcomes.
“It’s known that sometimes doing tissue biopsy can potentially cause initiation of different types of cancer,” Hong explains. “So that’s not really helpful. It’s painful, and you can’t take biopsies frequently, so the information we can get is fairly limited. And not every cancer is physically accessible, either.”
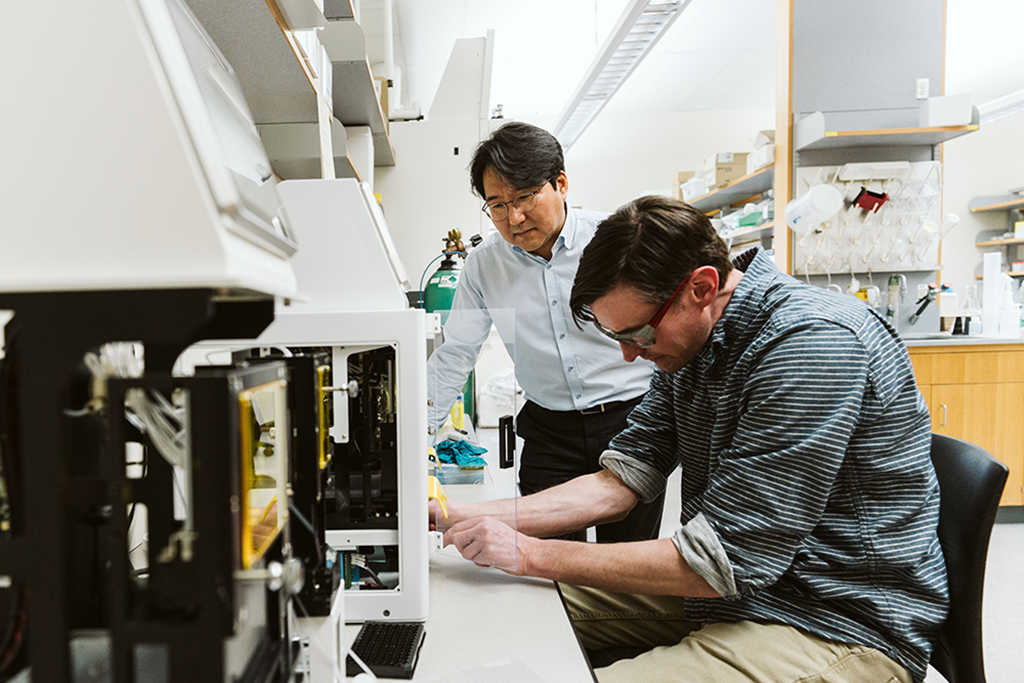
Although there is existing FDA-approved technology for CTC capture, it is limited in its effectiveness. To develop a better option, Hong’s lab looked to nature for inspiration, mimicking the same rolling mechanism that CTCs use to exit blood vessels and start secondary tumors away from the site of the primary tumor. Hong also leveraged the power of nanotechnology by incorporating CTC-specific antibodies that are immobilized inside nanoparticles, which then catch the CTCs as they tumble along.
“By doing that you can really enhance the local density of antibodies and then they can facilitate dramatically improving the binding strength,” Hong explains. “So now we can achieve much, much tighter binding using the nanoparticle-antibody combination compared to just the antibody alone, exponentially increasing the binding kinetics. That allows us to achieve highly sensitive and specific detection of CTCs.”
As a result, Hong’s method can capture up to hundreds of CTCs per milliliter of blood, compared to just single digits at best through the current FDA-approved system.
Putting new technology to the test
Clinicians from hospitals in Wisconsin, Iowa, Kansas, North Carolina, and Texas have turned to Hong’s lab to test the technology on blood samples from their patients. A small clinical trial with the University of Iowa recently showed that Hong’s CTC capture technology was able to accurately detect CTCs nearly 83 percent of the time in patients with gastrointestinal cancer and that the counts predicted disease progression three months after treatment. Those results were published in early 2023 in Biosensors and Bioelectronics.
Another clinical study at the University of North Carolina, published in late 2023 in the Journal of Clinical Oncology-Precision Oncology tested the method with patients whose cancer had started to spread (known as oligometastatic, an intermediate stage before cancer is widely spread). When researchers compared survival rates of those patients who had decreasing CTC numbers over treatments and those whose CTC numbers continued to climb, the results were statistically significant.

“That indicates that our CTC detection can be a strong indicator of disease progression,” Hong says.
Hong’s earlier preliminary research showed the method was also effective when used with patients with head and neck, lung, cervical, prostate, pancreatic, rectal, and renal cancers.
Because the technology is not yet FDA approved as a diagnostic tool, partnering clinicians still use standard monitoring methods to determine their treatment plans.
“It is purely the biomarker development right now,” Hong says. “But eventually we want to provide clinically useful information for the physicians to decide the best working treatment options for individual patients.”
Paving the way for clinical use
If all goes well with the next stage of research, Hong hopes to get FDA approval for in vitro diagnostics (use in human patients) in three to four years. But more funding could speed up that timeline. Capio Biosciences has secured approximately $4 million in investments, and the research has also been supported by government funding, from the U.S. National Institutes of Health and Korea. Hong’s team is also exploring partnering with a larger player in the diagnostics field.
“It’s challenging for a small biotech startup to bring a technology all the way from the beginning to the clinic,” Hong says. “There are a lot of things that we need to sort out, but if you find a bigger partner who has done that many times, then that’s going to make everything happen faster.”
“[This] indicates that our CTC detection can be a strong indicator of disease progression.”
—Seungpyo Hong
While the CTC capture technology is exciting on its own, Hong believes it is even more powerful when considered alongside other research underway in the School of Pharmacy — from colleagues who are designing new therapeutics to his own work improving drug delivery systems. Eventually, he hopes all the pieces work in concert.
“Those technologies are going to provide information really easily, by simple blood draw, on how this particular patient responds to a particular combination of treatments,” he says. “And then by doing that, we can really achieve truly personalized medicine. That’s the ultimate goal.”