11
September

Prestigious award recognizes three School of Pharmacy undergraduate students for their contribution to research
By Olivia Bouchard
On a campus with more than 35,000 undergraduate students, only about 100 are honored each year with a highly competitive research award: the University of Wisconsin–Madison’s Hilldale Undergraduate/Faculty Research Fellowship.
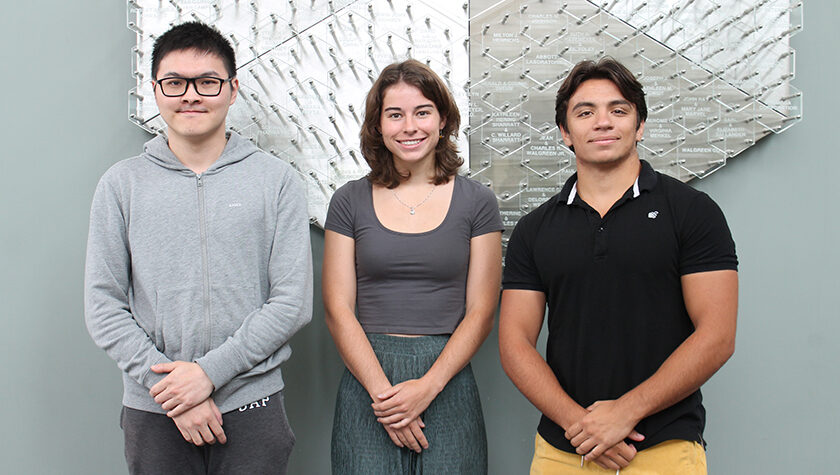
The UW–Madison School of Pharmacy’s undergraduate Pharmacology and Toxicology bachelor’s degree program has a long tradition of training successful researchers, and in the past five years alone, nearly 20 PharmTox students have earned the fellowship. This year is no exception: For 2023, UW–Madison selected PharmTox students Ethan Cui, Isabella Jones, and Adam Eckardt for the honor.
“I’m so proud of our students and their accomplishments — while all of our PharmTox students participate in research, receiving a Hilldale award is very prestigious, and it’s great that these students are being recognized for their work beyond the classroom,” says Kendra Gurnee, Pharmacology and Toxicology program coordinator.
“While all of our PharmTox students participate in research, receiving a Hilldale award is very prestigious, and it’s great that these students are being recognized for their work beyond the classroom.”
—Kendra Gurnee
The fellowship award celebrates undergraduates’ impactful original research and gives them a $3,000 stipend to further their research alongside their research supervisor. The fellows will also present their work at UW’s annual Undergraduate Research Symposium.
This year’s PharmTox award recipients are exploring issues from traumatic brain injuries to using oncolytic viruses as treatment.
Enhancing rehabilitation after traumatic brain injury
As traumatic brain injuries affect a staggering 70 million individuals annually and neurodegenerative diseases cast a shadow over the lives of around 25 million people globally, Cui is pursuing critical solutions through his research with Professor Jerry Yin, with the UW’s Laboratory of Genetics, and Associate Professor Grace Boekhoff-Falk, of the UW Department of Cell and Regenerative Biology.
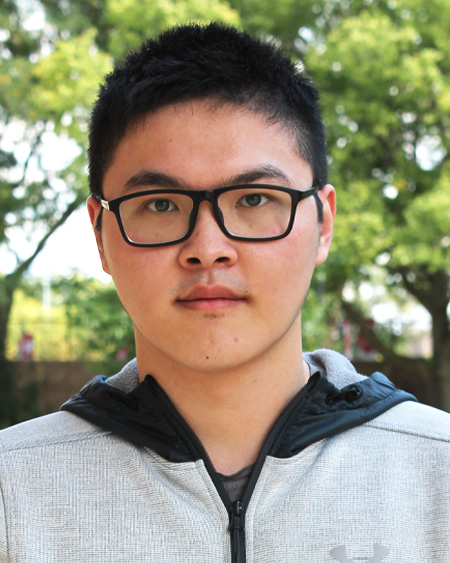
Cui says the inspiration for this research, which explores the unexpected link between traumatic brain injuries and social interaction, stems from a project he assisted with in Boekhoff-Falk’s lab.
“We unexpectedly found that the control group of flies with penetrative traumatic brain injury recovered faster in locomotor activity in a social housing context than the isolated housing context counterpart. Intriguingly, this difference in locomotor activity was not observed in the control group of flies without traumatic brain injury when placed in different housing environments,” says Cui. “This behavioral finding may potentially have significant implications within the field, linking it to key areas of research such as adult neurogenesis and neurodegenerative diseases.”
The research uses Drosophila, commonly known as fruit flies, as the model organism, because their genome makes a good human analogue.
Cui and his research mentors hypothesize that there may be mechanisms related to socialization that trigger neurogenesis, the growth and development of nervous tissue, that expedite the healing process. With support through the Hilldale Fellowship, Cui and his mentors will explore what those mechanisms might be.
This research is opening new doors to uncovering and comprehending certain principles of brain recovery to enhance rehabilitation.
Improving viral oncolytics
Human papillomavirus (HPV) and hepatitis B virus (HBV) are oncogenic viruses, or viruses that put a person at risk for cancer. With her research mentors, Jones is working toward a deeper understanding of the viral host genome interaction. Their research also dives into diseases that benefit from gene therapy treatments.

Jones is participating on a research team in the lab of Kinjal Majumder, with the UW Oncology Department, alongside graduate and undergraduate students from various programs including Microbiology Doctoral Training Program and Cancer Biology.
“My personal inspiration for pursuing this particular science stems from my excitement for molecular mechanisms,” says Jones. “I’ve been fascinated with infections and pathogens since the COVID-19 pandemic began in 2020, and viruses boast a unique capability to hijack host machinery that I’ve been eager to investigate.”
The goal of Jones’ research is to determine how multi-nucleotide mutation replication is regulated by DNA damage response proteins to improve viral oncolytics, which are a type of immunotherapy using viruses to target cancer cells. They are accomplishing this by looking into how MVM, an autonomously replicating parvovirus, restricts the host nuclei from taking over the DNA damage response proteins, which are vital in repairing DNA breaks that can be caused by cancer.
“My research with Hilldale funding will be focused on a further elucidation of MVM replication machinery and translating our past research into an application in oncogenic viruses such as high-risk HPVs,” Jones explains.
The aim of this research is to understand the molecular mechanisms of viruses that affect DNA to shed light on gene therapy vectors for the treatment of disease.
Treating ALS with stem cells
Each year in the United States, 5,000 people are diagnosed with amyotrophic lateral sclerosis, or ALS — a rare neurological disease that affects motor neurons, which are the nerve cells in the brain and spinal cord that control voluntary muscle movement.

Eckardt is working in Professor Masatoshi Suzuki’s lab in the Department of Comparative Biosciences to understand the early disease progression of ALS.
“The initial motivation behind my application to the fellowship was my commitment to researching ALS that I had made when my father was diagnosed with the disease way back in 2009,” says Eckhardt. “I became a part of Dr. Suzuki’s lab my freshman year and we recently came up with a new research direction that I applied to the fellowship with.”
Eckardt and Suzuki are hoping to uncover new mechanisms at the neuromuscular junction — skeletal muscle cells and motor neurons — that are linked to ALS disease progression and possibly more broadly motor neuron degeneration. They are using stem cell and rodent models to screen for drug targets linked to neuromuscular junction degeneration.
“In the long term, our goal is to develop new potential drug targets for ALS,” says Eckardt.