3
August

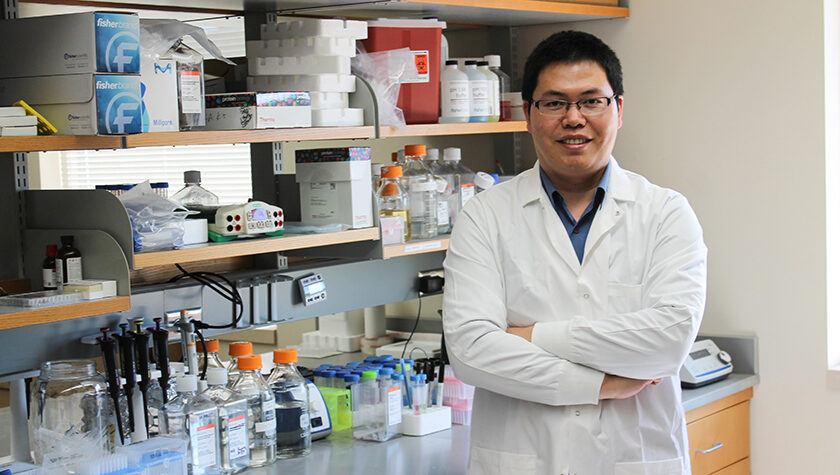
School of Pharmacy Assistant Professor Quanyin Hu and collaborators publish preclinical results on a new approach to prevent glioblastoma recurrence
By Nicole Sweeney Etter
Like the hardiest weed, glioblastoma almost always springs back — usually within months after a patient’s initial brain tumor is surgically removed. That is why survival rates for this cancer are just 25 percent at one year and plummet to 5 percent by the five-year mark.
One of the challenges of treating this disease is that surgeons can’t always remove every bit of tumor or glioma stem cells that might linger in the brain.
“One characteristic of glioblastoma is that the tumor cells are very aggressive, and they will infiltrate the surrounding tissues. So the surgeon can’t clearly feel the boundaries between the tumor and the normal tissue, and you cannot remove as much as possible because all the tissues in the brain are extremely important — you certainly don’t want to remove too much,” explains Quanyin Hu, an assistant professor in the University of Wisconsin–Madison School of Pharmacy’s Pharmaceutical Sciences Division. “So the tumor will come back again, and that sharply decreases the survival rate after treatment.”
But Hu’s Cell-Inspired Personalized Therapeutic (CIPT) Lab has developed a powerful immunity-boosting postoperative treatment that could transform the odds for patients with glioblastoma. The research by Hu and his collaborators was published in the August issue of the journal Science Translational Medicine.
“It provides hope for preventing glioblastoma relapse,” Hu says. “We prove that it can actually eradicate these glioma stem cells, which can eventually prevent the glioblastoma from coming back. We can significantly improve survival.”
Boosting antitumor immunity
Hu’s lab developed a hydrogel that can be injected into the brain cavity left behind by the excised tumor. The hydrogel delivery method works well because it completely fills the brain cavity, slowly releases the medicine into the surrounding tissue, and promotes the cancer-killing immune response, Hu notes.
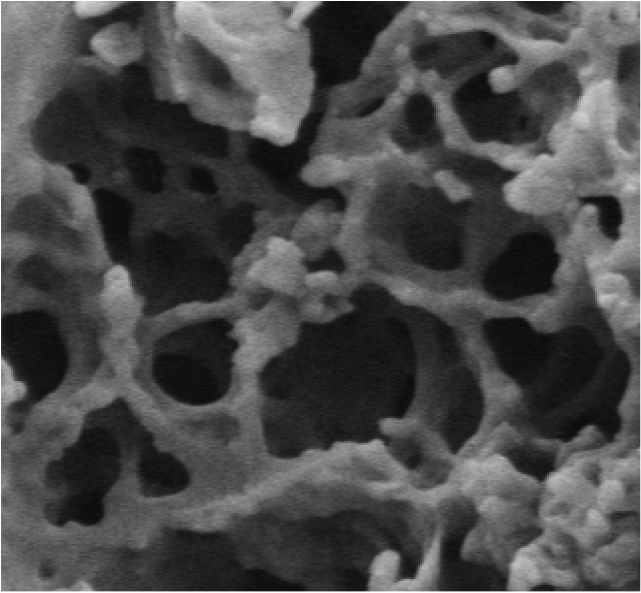
The hydrogel is packed with nanoparticles designed to enter and reprogram certain types of immune cells called macrophages. These immune cells normally clean up infectious invaders in the body, but in the tumor environment, they can change into a form that instead suppresses the immune system and promotes cancer growth. And because of the inflammation created by surgery, these rogue macrophages flock to the surgical site, potentially fueling cancer relapse.
“We want to take advantage of these macrophages and turn them from enemy to ally,” Hu says.
To do that, the nanoparticles can engineer the macrophages to target a glycoprotein called CD133, a marker for cancer stem cells. Hu’s team also added an antibody, CD47, that blocks a “don’t-eat-me” signal to promote macrophages to recognize the cancer cells. The preclinical results in mice models show that the hydrogel treatment successfully generated glioma stem cell-specific chimeric antigen receptor (CAR) macrophages — essentially engineering the immune cells on site to target and kill any lingering glioma stem cells.
If effective in humans, the hydrogel treatment could eliminate the need for postsurgical chemotherapy or radiation, reducing toxic side effects while also improving patient outcomes.
Paving the way for future research
Hu’s next step is testing the hydrogel in larger animal models and also monitoring long-term efficacy and toxicity beyond the four- to six-month period he previously studied.
“We have a lot of work to do before it can be potentially translated into the clinic, but we feel confident that this is a very promising approach for bringing new hope to patients with glioblastoma so they can recover after surgery,” Hu says. “We hope we can do our work to be able to advance this technology to the clinic.”
“We feel confident that this is a very promising approach for bringing new hope to patients with glioblastoma so they can recover after surgery.”
—Quanyin Hu
While Hu’s team is initially focused on glioblastoma, the treatment approach could also be applied to other aggressive solid tumors, including breast cancer, he notes. “Our approach is taking advantage of the macrophages in the postsurgical areas and to locally engineer these macrophages,” he says. “In this scenario, we can confidently say that it will apply to the majority of solid tumors with high invasive characteristics.”
Earlier this year, Hu published results in Nature Communications on a different cancer-fighting gel, a collaboration with School of Pharmacy Professor Seungpyo Hong and other colleagues in the UW School of Medicine and Public Health. Hu, who joined the UW–Madison School of Pharmacy in 2020, has found the university fertile ground for his research, especially as a young investigator.
“It’s the supportive, collaborative environment,” he says. “There are world-class scientists to help and support me. I was very fortunate to have this collaboration with physicians and scientists who get involved in clinical trials. That collaboration really shaped my thinking of how to make my research really impactful or feasible for the patient who is suffering from cancer or infectious disease.”




