Groundbreaking study from School of Pharmacy researchers reveals alarming misuse of OTC medications by older adults and offers a simple solution
By Andrea Mongler
A team at the University of Wisconsin–Madison School of Pharmacy recently conducted the first study to shed light on the extent of over-the-counter (OTC) drug misuse among older adults.
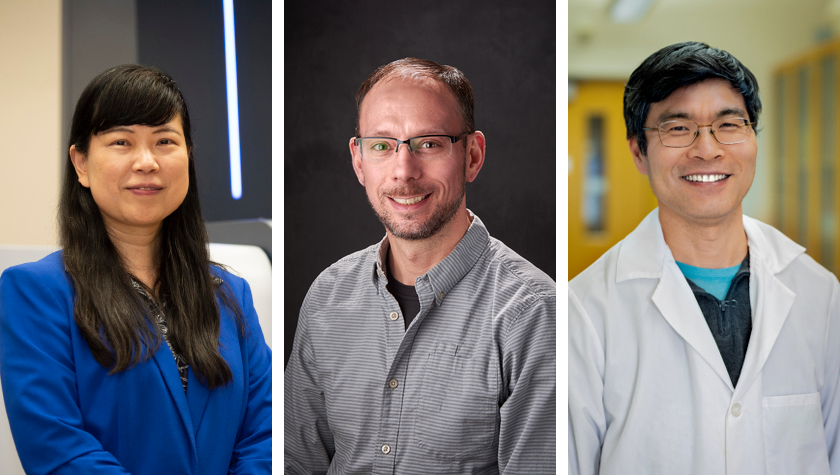
“We’ve known for years that OTC safety in older adults is a problem, but until now, we didn’t have evidence to demonstrate how serious this problem is,” says study co-author Michelle Chui, a professor of social and administrative sciences and director of the School’s Sonderegger Research Center for Improved Medication Outcomes.
The impetus for Chui and colleagues’ research dates back to 2014, when the Gerontological Society of America, in partnership with the Consumer Healthcare Products Association, published a white paper outlining an agenda for researching OTC use in older adults.

“The paper highlighted a patient safety gap in OTC misuse in older adults,” says Jason Chladek (PhD ’24), who worked on the new study as a graduate student in the School’s Health Services Research in Pharmacy program. “But there’s been almost no work in this area since then.”
The School of Pharmacy team’s groundbreaking study aims to fill that gap, finding that four out of five study participants demonstrated OTC misuse.
“This is a big deal,” says co-author Denise Walbrandt Pigarelli (BS ’91, PharmD ’93), associate professor of pharmacy practice. “I’ve been saying for years that OTC drug misuse in older adults is a major problem, and now we have evidence to support that.”
The good news? The team also developed a pharmacy-based intervention that successfully reduced misuse of OTCs linked to serious side effects in older adults.
The research
With a three-year grant funded by the Agency for Healthcare Research and Quality, Chui, Chladek, Pigarelli, and colleagues — including scientist Aaron Gilson, researcher Jamie Stone, and Associate Professor of Pharmacy Practice Ed Portillo (PharmD ’14) — partnered with Aurora Health Care to conduct a randomized controlled trial. The trial involved 288 older adults (age 65 and older) across 20 of Aurora’s community pharmacies in eastern Wisconsin.
Each study participant was asked to pretend they had been experiencing one of three types of symptoms: cough, cold, or allergy symptoms; pain (soreness and muscle aches); or sleep problems.
“We’ve known for years that OTC safety in older adults is a problem, but until now, we didn’t have evidence to demonstrate how serious this problem is.”
—Michelle Chui
Each participant chose one or more OTCs from the pharmacy shelves to treat these hypothetical symptoms. Researchers then asked participants how they’d use their OTC selections to treat their symptoms — and what they’d do if symptoms continued or got worse.
Ten of the 20 pharmacies were control sites, and the other 10 served as “Senior Safe” intervention sites, in which the researchers redesigned aisles containing OTC medicines. Specifically, they placed products that are safer for older adults between approximately shoulder height and knee height and moved higher-risk medicines out of easy reach — like the bottom shelf.
In addition, the team added green Senior Safe banners on the shelves to indicate medicines that are generally considered safe for older adults and red stop signs to indicate products considered high risk for them. Finally, the team moved some particularly high-risk products behind the pharmacy counter and added signs on the shelves to encourage patients to talk to pharmacy staff if they were interested in these products.
The prevalence of misuse
In a paper published in September in Innovation in Aging, Chui and colleagues described the findings of the control arm of their study — the 10 pharmacies that did not implement the Senior Safe intervention. They found that 79% of the 144 control participants demonstrated at least one type of misuse when describing how they’d use their selected OTCs after symptoms began.

“Finding such a high level of misuse was really surprising,” Chladek says. “It illuminated a serious patient safety gap that we need to proactively address.”
The most common types of misuse among participants were drug-drug (using a medication that interacted with another drug they were taking) and drug-label (not following label instructions). Thirty-eight percent of participants demonstrated misuse in two or more misuse categories.
When the 144 control participants were asked what they would do if their symptoms continued or worsened, 31 indicated they would use their initial OTC selection differently or add a new medicine. Of these, 74% indicated they would make a change that would lead to additional misuse.
“I hope this information gets incorporated into teaching at all schools of pharmacy and across health disciplines,” Walbrandt Pigarelli says. “If people understand the scope of the problem and work to address it, we can prevent many hospitalizations and so much morbidity.”
The successful intervention
In a second paper, published in October in the Journal of Patient Safety, the research team described the results of their Senior Safe intervention — and those results were equally striking.
“Senior Safe drastically reduced misuse in our test site pharmacies,” says Chui.
Specifically, for high-risk OTCs, intervention sites were 83% less likely to experience drug-drug misuse and nearly 64% less likely to experience drug-age misuse (using medications linked to increased risks for older adults) compared with control sites.
Notably, Chui says pharmacists and technicians were highly satisfied with the intervention.
“If people understand the scope of the problem and work to address it, we can prevent many hospitalizations and so much morbidity.”
—Denise Walbrandt Pigarelli
“It was critically important to us that not only does this intervention improve safety for older adults, but that it also does not increase workload for pharmacists and technicians,” she says. “We found that the conversations they were having with patients were more clinical in nature as opposed to them fielding questions about cost or where to find something, for example.”
The results of the intervention were so positive that Aurora Health has since implemented it across its 68 pharmacies in Wisconsin.

“Based on the results — the benefit to the patient, the benefit to the pharmacy team, and the low cost to implement — our leadership team supported rolling the intervention out system-wide without hesitation,” says Ken Walker, manager of retail pharmacy operations at Aurora Health Care, who worked closely with the School of Pharmacy team.
Chui says the researchers followed the additional pharmacy sites for three to six months after they implemented the intervention and found that the changes stuck.
“What often happens with these types of studies is that once researchers finish their work, the intervention sort of peters away to nothing — so the fact that Aurora Health Care has sustained the intervention shows us how doable this simple, effective change is,” says Chui. “Our hope is that other pharmacies nationwide will use this as an example and institute interventions of their own to improve OTC safety in older adults.”