A study led by School of Pharmacy faculty and students examines how Wisconsin pharmacies expand services but struggle with staffing, reimbursement
By Susan Lampert Smith
Many people witnessed how community pharmacists served as a lifeline during the COVID-19 pandemic, filling the need for testing, vaccinations, and other health care at a time when hospitals and clinics were overwhelmed and less accessible due to COVID restrictions.
Now, a new study from University of Wisconsin–Madison School of Pharmacy researchers highlights how community pharmacies in Wisconsin have expanded their services well beyond dispensing medications to meet the needs of patients who may live far from other health care providers, despite often not being reimbursed for their services.
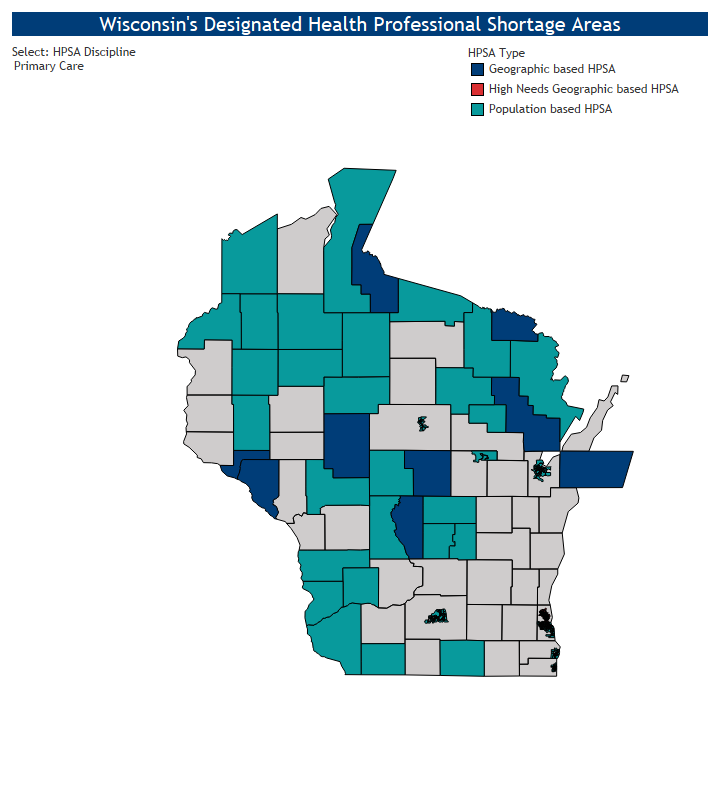
The study, led by Associate Professor Kevin Look (PharmD ’09, MS ‘11, PhD ’13), chair of the Social and Administrative Sciences Division, looks at the role played by community pharmacies in areas of Wisconsin’s health professional shortage areas (HPSAs), which are typically rural areas that lack adequate numbers of health care workers. A lack of accessible health care contributes to worse health outcomes for people living in these shortage areas.
“There’s this really great opportunity for pharmacists to take on this patient care role that our students want to do, that our pharmacists want to do, and that our communities need.”
—Kevin Look
“We knew there were a lot of innovative pharmacies in the state, but we didn’t really know how many, or where they were located,” he says. “What we found was a lot of uptake of newer pharmacy practice opportunities. There are a number of pharmacies who were leaders, on the cutting edge of these practices.”
Pharmacies as care access points
The study, published in the Journal of the American Pharmacists Association, included a survey of 287 Wisconsin community pharmacies in HPSAs. These pharmacies proved to be access points for care, reporting that they offer services such as compounding, blister packaging, medication therapy management, medication synchronization, comprehensive medication reviews, prescription delivery, and vaccinations.

A smaller number also leverage collaborative practice agreements to offer long-acting medication injections or contraceptive prescribing, and management for chronic conditions such as diabetes, hypertension, asthma, and chronic obstructive pulmonary disease (COPD).
Community pharmacies are uniquely situated to address these unmet health needs, says Look. About 90 percent of the U.S. population lives within five miles of a community pharmacy. The survey found that, regardless of location, pharmacies offered nearly the same breadth of services — with a slightly higher prevalence of non-dispensing services in HSPAs.
Penny Black, a rural epidemiologist with the Wisconsin Office of Rural Health and a study co-author, says the findings highlight the importance of community pharmacies in small-town Wisconsin.
“Community pharmacies are a critical healthcare access point in Wisconsin’s underserved communities,” Black says. “Rural areas have fewer clinics and hospitals than urban areas, and community pharmacies are accessible and trusted. Smaller populations in these areas allow pharmacists to build relationships with their patients and provide customized care.”
On the other hand, the study found that many of the community pharmacies were performing the services at a loss, reporting that the lack of reimbursement from private and government insurances and lack of staff were causing stress on their businesses. The survey found that the prevalence of reimbursement was less than 50 percent for two-thirds of pharmacies’ offered services.
“Pharmacies have this opportunity to meet the unmet needs, particularly in rural and inner-city areas, but a lot of them are doing it for free without getting paid for it, and that’s not a sustainable long-term practice,” says Look. “Our results show the tension between meeting unmet health care needs and making the pharmacy business sustainable and viable.”
Understanding rural health needs
Ed Portillo (PharmD ’14), associate professor in the School’s Pharmacy Practice and Translational Research Division and study co-author, says this work is an example of the research efforts led by PharmD students enrolled in the Rural Pharmacy Practice Program, who each take on a research project every semester.
“Some of the most innovative practice opportunities for pharmacists exist in rural communities,” Portillo says. “In the Rural Pharmacy Practice Program, students complete real-world rural healthcare projects that have a far-reaching impact beyond the classroom. Students are mentored by our alumni and serve as critical members of the healthcare team during their schooling. Actions of our students in the rural healthcare program truly exemplify the Wisconsin Idea.”
Madison Lee (PharmD ’22) was in the School’s recently launched rural health PharmD path in the fall of 2020 when the study launched as a class project.
“The idea started before COVID as ‘Let’s figure out what the community pharmacies are doing,’” Lee says. “Things got more interesting once COVID started because of the other services that started during the pandemic, such as testing and immunizations.”
Lee’s class — including study co-author Kelsey Rox (PharmD ’22) — identified the 774 community pharmacies in Wisconsin and helped create and pilot test the survey tool, which was then sent out by the next class of students — including co-authors Justin Arzt, Joseph Crahan, Mickaela Lucey, and Cara Helgeson, all fourth-year PharmD students — in November 2021 and March 2022.
The students received responses from 287, a response rate of about 37 percent.
By then, Lee was experiencing the practice innovations firsthand. She spent her fourth year at a Reedsburg community pharmacy as part of the rural-focused Residency Track Advanced Pharmacy Practice Experiences, where she did comprehensive medication reviews with patients and counseled them on staying up-to-date with their immunizations.
“During COVID, patients were really appreciative of what we were doing,” she says.
Meeting community needs
Today Lee splits her time between the Aspirus Divine Savior Hospital pharmacy in Portage, while still working as a per diem pharmacist at the Reedsburg Area Medical Center. She sees the need for new pharmacy services to improve the health of patients.

“For example, if patients come into the hospital with poor adherence to their medications, I will often recommend bubble packing, because it packages all their morning meds, and all their night meds, and helps them take the correct medications at the correct time,” she says. “It keeps things as organized as possible, especially for older adults who may have 10 or 15 medications. If they get admitted to the hospital, they can bring the bubble packs with them and we’ll know exactly what they’re on.”
The study also helps paint the picture of pharmacy practice in underserved areas of Wisconsin at a time when state law is changing. During 2024 Wisconsin Act 98 will go into full effect, which directs the state Medicaid program, serving low-income families, to reimburse pharmacists for services that are within their scope of practice.
Look says he believes the Wisconsin survey of community pharmacies can help inform broader policy discussions that are going on at the state and national levels. For example, community pharmacies in the study cited staffing issues, time stress, and financial issues as barriers to expanding their services to meet the needs of their patients.
“There’s this really great opportunity for pharmacists to take on this patient care role that our students want to do, that our pharmacists want to do, and that our communities need,” Look says. “But without a mechanism in place to make it financially viable, we’re not going to have those services … action is needed to support community pharmacies so they can meet the needs of their communities.”
