
New research by School of Pharmacy Professor Lingjun Li uncovers the role of neuropeptides in post-traumatic stress disorder
By Nicole Sweeney Etter
Post-traumatic stress disorder (PTSD) is often associated with veterans who have experienced the horrors of war, but the condition can be triggered by a wide range of traumatic events. It’s estimated that 6 percent of the U.S. population will experience PTSD at some point in their lifetime, according to the National Center for PTSD.
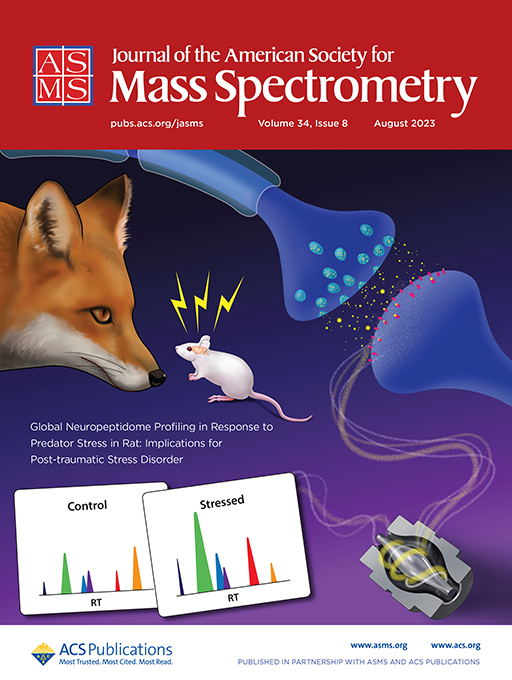
And there’s vast room for improvement in PTSD care. That’s why University of Wisconsin–Madison School of Pharmacy Pharmaceutical Sciences Professor Lingjun Li teamed up with Vaishali Bakshi, an associate professor in the Department of Psychiatry, in the first study to take a comprehensive look at the neuropeptides potentially involved in PTSD. The team’s research was recently highlighted on the cover of Journal of the American Society for Mass Spectrometry (cover art designed by Sally Griffith-Oh of the School of Pharmacy).
Li, the Charles Melbourne Johnson Distinguished Chair and the Vilas Distinguished Achievement Professor of Pharmaceutical Sciences and Chemistry, is known for her innovative work designing tools to better understand neuropeptides, a class of key chemical messengers in the brain. Now she’s using that expertise to illuminate new possibilities for patients with PTSD.
“Sometimes PTSD is not correctly diagnosed,” Li says. “There are limited drugs or clinical treatment options, and they’re not very effective. And I think that’s in part because we still don’t have a full understanding of all the underlying neural chemical or neural molecular mechanisms that could lead to PTSD. I think it’s reasonable to hypothesize that a lot of these different peptides play a role.”
The research question: How do neuropeptides change in response to traumatic stress? To find out, the team looked at five fear-circuit brain regions believed to play a role in PTSD. That includes the basolateral amygdala, which processes threat-related stimuli; the prefrontal cortex, which is involved in the extinction or retention of fear; the hippocampus, which helps with memory processing, context, and coding; the hypothalamus paraventricular nucleus, which is involved in managing the demands of chronic stress exposure; and the nucleus accumbens, which has been implicated in regulating stress-related behavior.
Li wanted to look at the neuropeptide content in those regions before and after rats were exposed to predator-induced fear, which could mimic the human response to a traumatic event.
What they found: The research team identified more than 600 neuropeptides involved in the stress response.
“Some of these are from well-known peptide families that also appear to be involved in regulating the PTSD response,” she says. “Not only that, but they also achieved that in a brain region-specific manner, which is actually a great interest for neuroscience because we know that the brain is a very heterogeneous structure. Different parts of the brain could have the same peptides, and depending on where those peptides are expressed, they may have quite different functions. Using our high-resolution mass spectrometry instrument, we can actually look at those details.”
Why this matters: There are still many gaps in our understanding of PTSD and how to effectively treat it. Researchers already have a basic understanding of other neurotransmitters, including dopamine and gamma-aminobutyric acid (GABA), that are involved in the stress response.
“But there is much less knowledge about the neuropeptides involved,” Li says.
Other research has shown that certain neuropeptides, including corticotropin-releasing factor (CRF) and some opioid peptides, play a role in PTSD. But Li wanted to study a much larger array of neuropeptides.
“One of our goals is to hopefully see some new bioactive peptides because the previous treatments are not effective or are less efficient,” she says. “If the treatment is not effective, then that would implicate other molecules or molecular pathways that we should be looking at.”
The study also found well-known peptides, such as cholecystokinin (CCK) and neuropeptide Y, that are already targeted by existing pharmaceutical treatments for other conditions. Because this is the first time those peptides have been identified as playing a role in traumatic stress, it could open up new applications for existing drugs.
What researchers learn about PTSD could also be helpful for other conditions that include an imbalance in peptides, including neurodegenerative diseases and other brain disorders like drug abuse.
How they did it: To create an animal model of post-traumatic stress, researchers in the Bakshi Lab exposed rats to fox urine to trigger their instinctive predator fear. Rats in the control group were fed a regular diet while the other rats had the stress-inducing fox urine mixed into their food.
The brain cells of the stressed rats released neurochemicals that triggered a downstream response. After extracting the neuropeptides, Li and her research team analyzed them in a mass spectrometer.
“The key to our method is employing high-resolution mass spectrometry to measure these peptides and not only look at their identity, but also measure their relative abundance,” Li said. “This really expands the chemical complexity that you can look at.”
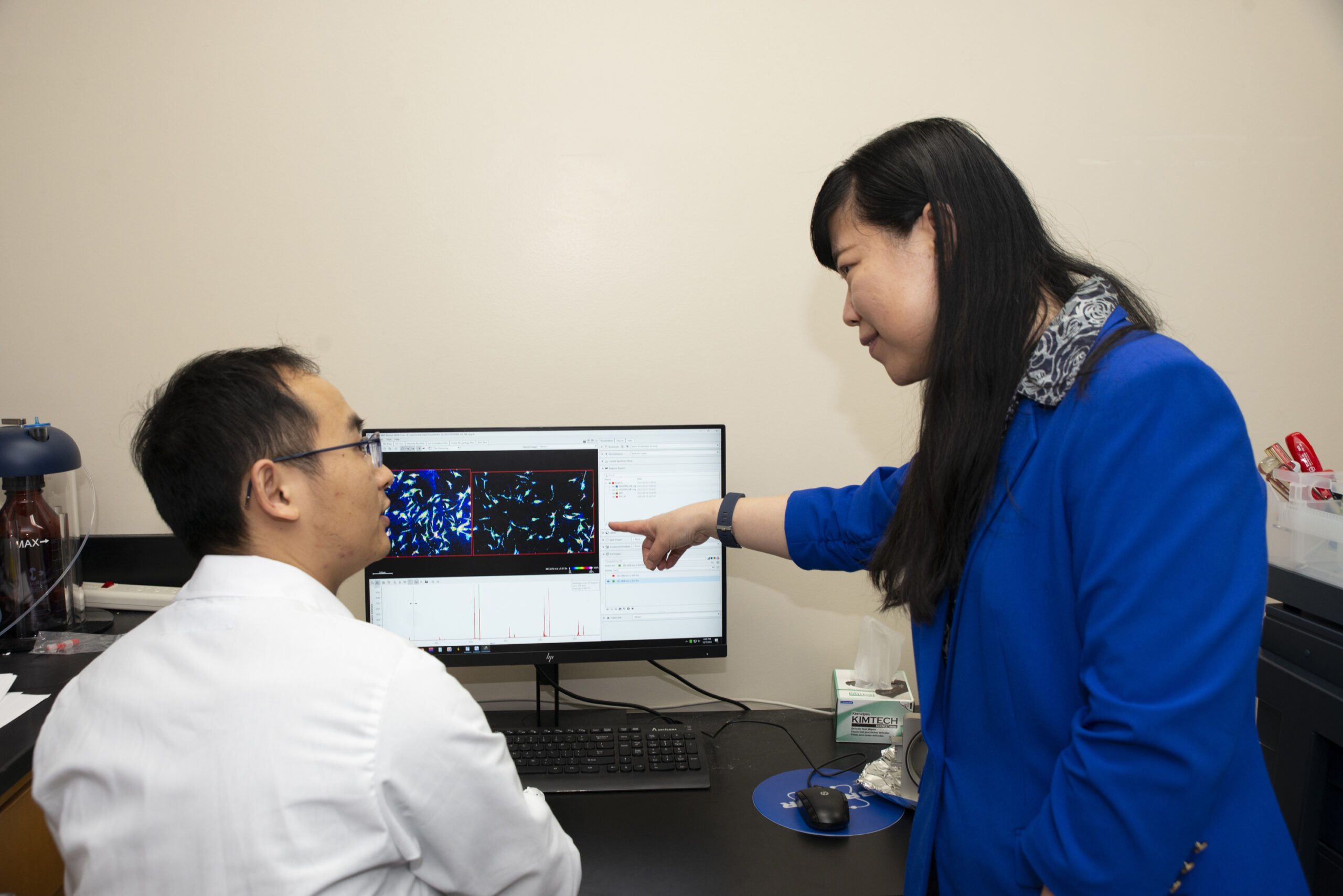
The research team used statistical analysis to determine how different peptides are changing across brain regions and which seem to be the most significant. This work was co-led by graduate student Wenxin Wu and postdoctoral researcher Min Ma, in collaboration with two other graduate students, Angel Ibarra and Gaoyuan Lu, in the Li Research Group.
What’s next: While the initial study looked at brain regions more widely, Li could use mass spectrometry imaging technology to drill down to the single-cell level to learn even more. Researchers can then look more closely at the neuropeptides they’ve identified at the neural circuit level to see if they might be biomarkers that could improve PTSD diagnosis or be used as novel therapeutic targets.
Male and female rats had different types and levels of neuropeptides after exposure to traumatic stress, so Li also hopes to further explore the sex differences.
“There are a lot of possibilities for future experiments,” she says. “We’re only scratching the surface of this, but I think mapping out different pathogenic pathways and analyzing the crosstalk between different neuropeptides could really impact our understanding of PTSD and other stress-related disorders and ultimately lead to better treatment.”
