Assistant Professor Marina Maes aims to assess how the overturn of Roe v. Wade has affected Wisconsin pharmacists’ perceptions of their role in providing reproductive health care
By Brianna Foth
Earlier this year, the U.S. Supreme Court overturned a nearly 50-year precedent cementing the right to abortion. In the wake of this ruling, providers dealing in reproductive healthcare are scrambling to understand new regulations, and contraceptives have become the focus of many conversations — in particular, emergency contraceptives.
Like many healthcare practitioners, pharmacists are left to wonder what’s expected of them and how they can best use their expertise to serve their patients in a post-Roe world.
“The overturn of the Roe v. Wade Supreme Court case is likely to have some downstream effects on how pharmacists perceive their role in providing reproductive health care services to patients,” says Marina Maes, assistant professor in the University of Wisconsin–Madison School of Pharmacy’s Pharmacy Practice and Translational Research Division.
“The overturn of the Roe v. Wade Supreme Court case is likely to have some downstream effects on how pharmacists perceive their role in providing reproductive health care services to patients.”
—Marina Maes
To illuminate some of these effects, such as the intention, expectation, and ability of pharmacists to provide reproductive healthcare services, Maes is launching a survey directed at Wisconsin pharmacists.
“What I’m interested in looking at is whether this overturn of the Supreme Court case has impacted pharmacists’ knowledge, attitudes, or comfort with providing reproductive health care services,” she says. “Ultimately, this study is geared toward helping us design interventions that will help pharmacists to provide these important services to patients.”
Assessing abilities and intentions
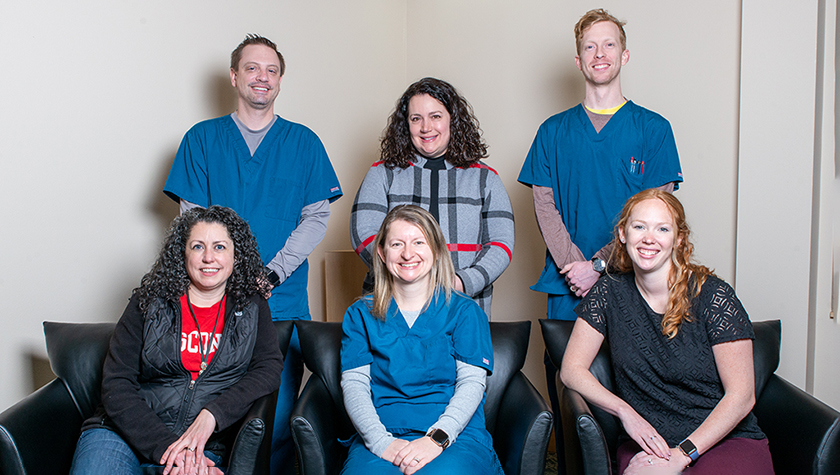
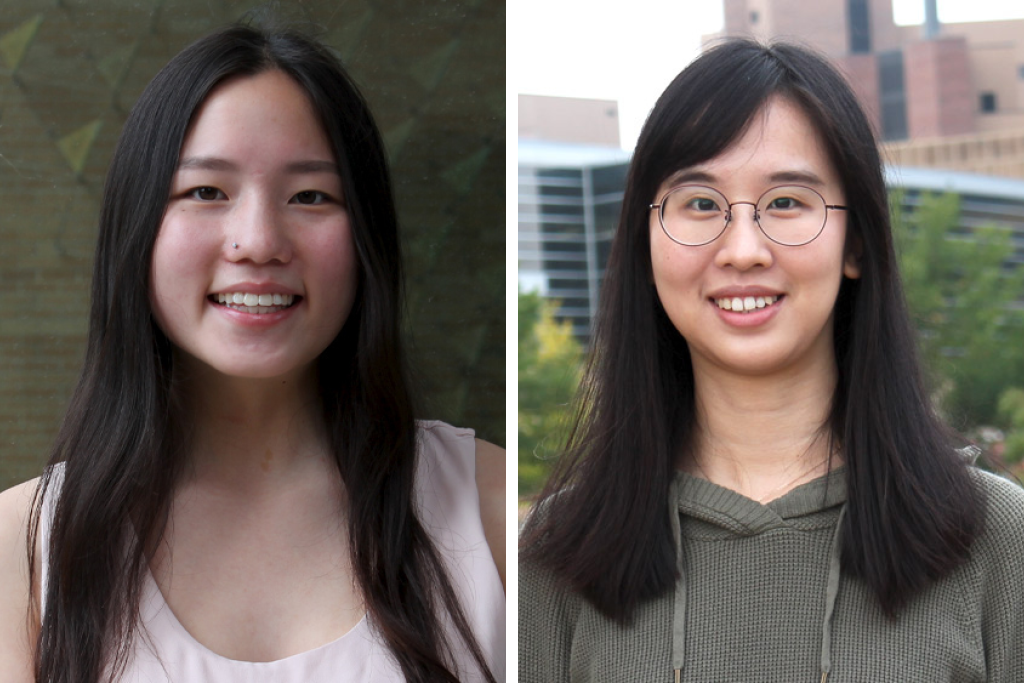
Along with Health Services Research in Pharmacy graduate student Meng-Jung Wen, PharmD student Joyce Hu, and Concordia University’s Kassandra Bartelme, Maes is designing the survey to follow the Integrated Behavior Model, a framework for understanding human behavior that proposes that behavior is most likely to occur if a person has a strong intention to perform it and the knowledge and skill to do so.
Many of the survey’s questions, therefore, will revolve around learning more about pharmacists’ intention to provide reproductive health care services, which falls into three domains: education and counseling on prescription and non-prescription contraception available through community pharmacies, access to and education about over-the-counter and prescription emergency contraception, and connecting patients with additional resources for reproductive healthcare. Those resources can include information about contraceptives and emergency contraceptives that are not available through the pharmacy; referrals for more comprehensive women’s health services, such as pregnancy testing or a pelvic exam, or to community resources like Planned Parenthood.
The survey will also explore their perceptions of their own knowledge and skills, in order to predict how likely they would be to continue providing these services now and to expand services in the future.
“If we can identify what’s impacting their ability to provide the services, then we can design an intervention that would help to improve pharmacists’ knowledge and skills,” says Maes.
The team plans to disseminate the survey through the Pharmacy Society of Wisconsin (PSW), whose membership includes roughly 900 community pharmacists in the state of Wisconsin. Then, the team will be conducting follow-up interviews with a sample of the respondents to learn more about how environmental factors may have played a role in their responses. The sample of pharmacists for the follow-up interviews represent perspectives from different geographic regions and different types of community pharmacies.
“There are factors within the pharmacy itself or within the pharmacist’s geographic region that can limit them in doing certain things. Is it expected by patients that pharmacists are providing these services? Is it expected by other health care providers? Is it something common in their practice?” says Maes. “If pharmacists have already provided these services for a long time, they’re more likely to continue to provide them.”
“If we can identify what’s impacting their ability to provide the services, then we can design an intervention that would help to improve pharmacists’ knowledge and skills.”
—Marina Maes
Maes also aims to assess whether media coverage of the Roe v. Wade overturn may have served as an additional environmental factor in shaping pharmacists’ attitudes or approach toward reproductive health.
“We’ll survey pharmacists to evaluate their knowledge and attitudes towards the provision of reproductive health care services more generally, and then specifically following the overturn of Roe v. Wade,” says Maes. “The goal is to cast as wide a net as possible for the initial survey, and then do follow-up interviews to gain more information. Using this mixed methods approach can really help to further explain what we’re seeing.”
A clinical need
With this study, Maes was initially aiming to understand pharmacists’ perspectives on legislation proposed in Wisconsin that would allow pharmacy providers to directly prescribe and dispense self-administered contraceptive methods, such as the pill, patch, ring, or shot.

Although the bill was passed by the Wisconsin State Assembly in 2021, it failed to reach the state Senate before the end of the 2022 legislative session. And when Roe v. Wade was reversed, Maes saw an opportunity to understand the critical role of pharmacists in reproductive health.
In her clinical practice at the UW Health Belleville Family Medicine Clinic, Maes often fields questions related to contraceptives and reproductive health.
“I get a lot of questions like: ‘My patient is having a side effect with this contraceptive, what should we choose instead?’ And often, patients just stop taking their medication altogether, which could really increase the risk of unintended pregnancy,” she says.
In practice, physicians may only get to spend 10 or 15 minutes with a patient in an office visit. In the case of prescribing contraceptives, that may not be enough time tell patients about what their options are for emergency contraception and what to do if they miss a dose.
“There are a lot of opportunities for pharmacists to fill that information gap to help prevent unintended pregnancies.”
—Marina Maes
“There are a lot of opportunities for pharmacists to fill that information gap to help prevent unintended pregnancies,” says Maes.
Unintended pregnancy, she explains, can have significant health implications for both the mother and the developing fetus. Women experiencing unplanned pregnancy are both less likely to seek early prenatal care and at a higher risk for developing postpartum depression. Unintended pregnancy has also been associated with higher rates of preterm birth and low birth weight, which can be predictors of health problems later in life.
“Pregnancy is not always a safe thing to experience,” says Maes. “So, reducing unintended pregnancy is important. And providing adequate access to contraception and education about contraception is an important way to help reduce unintended pregnancy.”
In the classroom
Maes’ work in reproductive health also transcends her clinical practice, making its way into the classroom.
“When pharmacists or pharmacy students are confident in their skills, it can help them provide adequate education to patients and to know what resources are available to them,” says Maes. “We also want to ensure that our student pharmacists can educate patients in a way that’s culturally sensitive and inclusive, because there are so many different identities and experiences that can create different views on contraception and family planning.”

In keeping with that idea, Maes recently designed a comprehensive women’s health lab to prepare pharmacy students to prescribe contraceptives and to also approach contraceptive care in a way that’s both inclusive and culturally sensitive. For that project, the American Association of Colleges of Pharmacy Laboratory Instructors Special Interest Group honored Maes with a Laboratory Innovation and Teaching Excellence (LITE) Award.
“It’s important that our pharmacy students know how to interact with diverse patients and that they feel comfortable doing so,” says Maes. “There’s an inherent bias or assumption that somebody who’s using contraception is taking it to prevent pregnancy; however, that individual could be not sexually active, or they could be sexually active with a partner who could not physically get them pregnant.”
Although pharmacists do not currently have prescriptive authority for contraception in the state of Wisconsin, she believes it’s still important to prepare her PharmD students at the School of Pharmacy for a possible future in which they can. After graduation, these students will play an important part in advocating for expanded pharmacist roles including contraceptive prescribing, she says.
“Pharmacists are an important contact point to provide patients with resources to access contraception and emergency contraception, even if they do not have prescriptive authority yet,” she says. “But I think it’s still important for our student pharmacists to be prepared to provide that service when it is passed, or if they go on to practice in another state that has the legislation. They should be well-equipped and prepared to be able to prescribe contraception.”