15
June

Clinical services and ambulatory care grow as workforce becomes more diverse
By Katie Ginder-Vogel
More pharmacists are providing clinical services, and the field of ambulatory care is growing. The workforce is becoming younger, more educated, more diverse, and more gender-balanced. These are just a few of the positive trends identified by the 2019 National Pharmacist Workforce Study, a national survey of pharmacists conducted every four to five years that was launched at the University of Wisconsin–Madison School of Pharmacy.
The report is sponsored by the Pharmacy Workforce Center, a coalition of non-profit pharmacy organizations whose mission is to serve the pharmacy profession and the public by actively researching, analyzing and monitoring the size, demography, and activities of the pharmacy workforce. The members of the research team are representatives of their respective academic institutions and collaborate as the Midwest Pharmacy Workforce Consortium.
“There is a strong UW influence on the workforce study group,” says research team member and School of Pharmacy Professor Dave Mott (BS ’88, MS ’92, PhD ’95), William S. Apple Distinguished Chair and chair of the Social and Administrative Sciences Division. He was on the original research team, which started as a grassroots effort at the School of Pharmacy, as a graduate student, with his advisor Professor Emeritus David Kreling, who continues to work on the report.
Mott’s former School of Pharmacy classmates Bill Doucette (BS ‘83, PhD ‘93), a professor at the University of Iowa College of Pharmacy, and Jon Schommer (BS ’85, PhD ‘92), a professor at the University of Minnesota College of Pharmacy, are also on the team.
“We need to do a better job of highlighting the areas [of pharmacy] that are growing, so we can share that with students and alumni.”
—Dave Mott
“I’ve been doing this workforce study almost my whole career,” says Mott. “It’s a wonderful group of people. We’ve known each other for a long time and like working together.”
Additional authors include Caroline Gaither (University of Minnesota College of Pharmacy), Brianne Bakken (Medical College of Wisconsin), Matthew Witry (University of Iowa College of Pharmacy), and Vibhuti Arya (St. John’s University).
“We set out to answer a bigger set of questions than we had in the past,” says Doucette. “Because it was an online survey, we could use branching and skipping to tailor sets of questions to subgroups of respondents for the first time.”
This year’s report looked at data from the past 20 years and noted three key positive trends: an increase in clinical activities performed by pharmacists, growth in ambulatory care, and more diversity in the profession.
Trend #1: Growth in clinical services
In a section of the survey about work activities, the research team asked pharmacists to break down the portion of their time they spend on different activities, and the results showed more pharmacists moving into the clinical realm.
“Product distribution and dispensing activities have been the pharmacist’s bread and butter for a long time, but in the last 20 years or so, we’ve gotten more into clinical activities,” says Doucette. “We found that more pharmacists are spending more time on non-dispensing care activities, like medication management — working with patients and prescribers to make sure there are no problems with medications, so they’re safe and effective.”
The result is that patients have an additional care provider who is accessible, especially if that provider is a community pharmacist, many of whom provide services like medication consultations, vaccinations, and medication-assisted therapy for substance misuse.
“It’s good for patients and providers to have another professional seeing the patient who knows what medications they’re taking,” says Doucette. “It’s a win for pharmacists as well because their PharmD degrees prepare them to provide clinical services and practice at the top of their license, which is intrinsically rewarding and good for pharmacists.”
Doucette also noted the importance of the Community Pharmacy Enhanced Services Network (CPESN® USA) business strategy: provide a breadth of services to increase patient care along with revenue.
“If we can get provider status — getting payers to recognize and be willing to pay for services we provide — that would be good for patients, providers and payers,” says Doucette.
In the conclusions of the report, the authors noted that the availability of payment for enhanced services plays a major role in the number of pharmacists who are delivering them. Mott would like to further examine the trend.
“If more pharmacists are doing direct patient care, we need to find out where those sites are and study those places to figure out strategies and best practices to expand that,” says Mott. “We need to do a better job of highlighting the areas that are growing, so we can share that with students and alumni.”
Trend #2: Growth in ambulatory care
As clinics move toward value-based payment and the use of metrics related to medication use to determine reimbursement amounts for pharmacists, it’s helpful to have pharmacists on staff who can attend to the drugs reflected in those metrics and make sure people are getting tested, keep their levels in range, and adhere to their medications.
“Pharmacists can’t bill independently for services, so until they get federal provider status, clinics will be mixed about going that route,” says Doucette. “But it’s positive that there’s growth.”
The workforce report’s findings about the increase in ambulatory care are consistent with the Bureau of Labor Statistics’ report, which projected flat job growth in pharmacy from 2018 to 2028. However, jobs within the field are simply shifting to more patient care-oriented areas — such as ambulatory care, outpatient/clinical pharmacotherapy — and away from dispensing roles.
Trend #3: Greater diversity in the profession
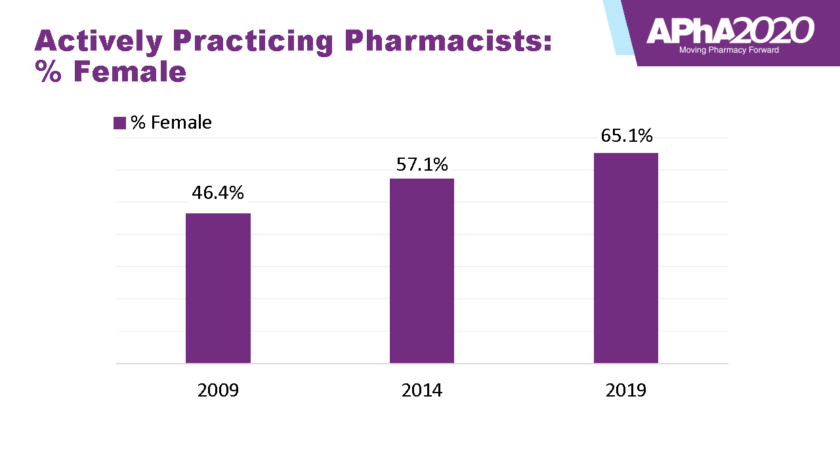
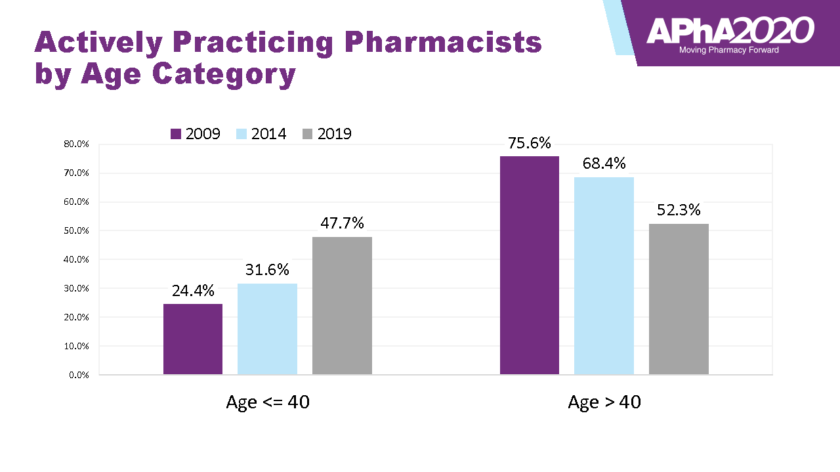
The study’s conclusions brought up some new findings, like increases in pharmacists of color, female pharmacists, and pharmacists under 40. These areas will be important to monitor, says Mott.
“The workforce is getting younger,” he says. “Younger pharmacists are well-trained and continuing on to do residency training. The profession is well-positioned to play a bigger role in health care.”
“Growth in diversity and women in the profession helps us better match our patient population,” says Doucette. “We’ve been deliberate about admitting diverse PharmD classes and expect that growth in diversity to continue. We will continue to monitor that by tracking basic demographics.”
The percentage of white pharmacists deceased by nearly seven percentage points between 2014 and 2019. In particular, the proportion of black pharmacists saw the most growth, more than doubling within the same time frame. Women now comprise over 65 percent of actively practicing pharmacists, and the report reflects an increasing number of women in management, representing 58.8 percent of managers.
“In the report, over half of the management professionals who responded are female,” says Doucette. “It’s good to have women in those positions to more fully reflect the makeup of the profession.”
Mott says the research team is aware of the need to modify their survey instrument to expand demographic questions, so people can more accurately classify themselves.
“We need to monitor these trends and implement programs at the pharmacy school level to increase recruitment and enrollment of more diverse students,” he says. “I’m hopeful that our report will lead to initiatives to increase enrollment of more diverse students, leading to a more diverse profession.”
Perceptions of leadership
This year’s survey included a new section about leadership. The research team explored attitudes about pharmacy leadership by sending pharmacy administrators, owners, and managers a set of questions about succession.
“We included standard questions about people’s positions and tasks, but we had a big section where we asked people about leadership,” says Mott. “We wanted to gauge their perceptions about the quality of the pipeline to fill leadership roles.”
Another set of questions asked staff pharmacists about their interest in becoming leaders or managers: How interested are you? What would make you interested? Why aren’t you interested?

“We asked people not in leadership yet if they had received offers to lead and whether they had accepted,” says Mott. “Do they feel qualified or have concerns? There’s pretty good recent literature about a leadership void, so I think it’s helpful to get a sense of what’s out there and whether we have young pharmacists who want to do it or not — and if not, why?”
What they found was a reasonable, but not overwhelming, interest. The survey also asked what type of leadership was most appealing, and mentoring was a popular response.
“They felt that was a less formalized way of leading, maybe because it doesn’t include the difficult parts of being a manager, like resolving conflicts, budgeting, or working extra hours,” says Doucette. “How can we support pharmacists already doing that with resources?”
Doucette says pharmacy schools and associations are useful resources for cultivating leadership skills in students and alumni. “Pharmacy association national meetings try to make it easy for students to attend, with lower fees, special programming, and leadership training woven in,” says Doucette.
Mott says the School of Pharmacy’s non-credit Pharmacy Leadership Certificate and Mentor (LCM) program helps PharmD students develop leadership skills.
“Students can track into a leadership certificate program that pairs students with mentors and incorporates reflection, self-awareness, and Social Emotional Learning skills,” says Mott. “It gives students exposure to a mentor who’s a good leader and gets them thinking early on about leadership and what it means to be a good leader. We plan to continue to monitor where our graduates go, and hopefully, we’ll see an even larger proportion of them in leadership roles.”
Understanding burnout
Doucette says the research team plans to do further exploration on one finding: pharmacists at big national chains had greater levels of burnout and lower levels of fulfillment.

“It’s not really a trend; it’s a finding,” he says. “It’s not a high level of burnout. This is the first year we’ve measured this, and the overall mean is OK, and if you look at the metrics separately, it’s still not at an alarmingly high level, but we will keep an eye on it and do more exploration of what is really happening — more monitoring and more study of groups at risk for burnout.”
The researchers can further explore levels of burnout by analyzing the data they collected to see which other variables factor in, or they can include it in each future workforce exploration study and measure trends.
“After the study, we talked about the fact that it is super important to learn from the environments in which our alumni are working, to find out what our alumni are doing,” says Mott. “We should identify practice settings that are operating under best practices to make the environment better for pharmacists and learn from them. What are they doing that keeps their pharmacists happier? That’s really important.”
A closer look
“We came up with probably 10 papers to write over the next five years,” Doucette says. “We typically publish a half dozen additional peer-reviewed publications based on this study.”
One big follow-up topic that Mott plans to explore connects to questions about growth in the field of pharmacy.
“We need a better way to measure the status of demand for pharmacists: Is there a surplus or shortage? We need a better way to measure that,” says Mott. “That’s the next big thing we need to do.”
Mott and Brianne Bakken are working on a similar survey for the state of Wisconsin. “Brianne has done a good job of taking our national, email-based survey instrument and modifying it for use in Wisconsin,” says Mott. “We aim to get it out this summer and disseminate the results quickly.”
The group hopes to be able to share results of the Wisconsin study this fall.
“This is an exciting, yet challenging time in the profession,” says Mott. “As pharmacists continue to gravitate toward direct patient care roles and practice at the top of their license, challenges include receiving fair payment for services and figuring out, from an operations perspective, new models to provide the services. It’s exciting because many of our alumni are in leadership positions working on these issues every day.”